Abdominal cocoon in a young man
Department of Surgery, Government Medical College and Hospital, Chandigarh, India
Corresponding Author:Robin Kaushik, Email: robinkaushik@yahoo.com
Abdominal cocoon in a young man
Mayank Jayant, Robin Kaushik
Department of Surgery, Government Medical College and Hospital, Chandigarh, India
Corresponding Author:Robin Kaushik, Email: robinkaushik@yahoo.com
BACKGROUND:Intestinal obstruction remains a common problem encountered in the surgical emergency, and usually occurs secondary to adhesions, obstructed herniae or tubercular strictures. However, at times, rare causes of obstruction can also be encountered.
METHODS:A 24-year-old male patient presented with recurrent episodes of intestinal obstruction that was found to be secondary to an abdominal cocoon on laparotomy.
RESULTS:The patient underwent adhesiolysis of the cocoon, and remains well on a follow-up. Histopathological report of the cocoon wall revealed fi brocollagenic tissues with a mixed in fl ammatory in fi ltrate, without any evidence of tuberculosis.
CONCLUSIONS:Abdominal cocoon can be a rare cause of intestinal obstruction in male patients. Adhesiolysis of the cocoon membrane releases the obstruction and gives good results.
Intestinal obstruction; Cocoon; Idiopathic; Tuberculosis; Emergency surgery; Laparotomy
INTRODUCTION
Intestinal obstruction is seen frequently by surgeons all over the world. Commonly, adhesions and bands are implicated in developed countries, whereas obstruction of inguinal hernia and tuberculosis of the gastrointestinal tract are the common offenders in the developing countries.[1]The 'cocoon' remains an obscure and relatively uncommon cause of intestinal obstruction that is seen more commonly in females, wherein the intestine is encased in a thin, semitransparent membrane that causes obstruction by mechanical compression and kinking of the intestine loops contained within.[1–5]
We report the case of recurrent intestinal obstruction in a young male patient that was secondary to an abdominal cocoon and was managed successfully in our hospital.
CASE REPORT
A 24-year-old man was admitted to the hospital with recurrent episodes of abdominal pain, vomiting and constipation over the past six months. He had been taking symptomatic treatment from his local doctors with near complete resolution of symptoms every time. This time, however, he remained symptomatic, with persistent vomiting and constipation. A contrast enhanced computerized tomogram scan (CECT) of the abdomen showed distended small bowel loops, more localized to the left upper quadrants, but without any apparent cause of obstruction (Figure 1). As his symptoms did not resolve, he was referred to us and we planned to take him up for surgery.
Laparotomy was performed by a midline incision. On entering the abdomen, the bowel loops were seen encased in a thin membrane (Figure 2) that completely covered the small bowel, ascending and transverse colon, stomach, and even going up to encase the spleen. Gently, with great care, adhesiolysis of this membrane was done and the whole of the bowel was freed, right from the duodeno-jejunal fl exure up to the ileo-cecal junction. Part of the cocoon that encased the colon and stomach was also released, and the patency of the bowel lumen was checked by milking the intestinal content into the colonand seeing that it passed freely right up to the sigmoid colon.

Figure 1. CT scan image showing dilated small bowel loops.
The post-operative period was uneventful, and the patient remains well on a follow up. We questioned our patient in the post-operative period about any possible etiological cause, but could not find anything in his history to suggest a 'trigger' for the formation of the cocoon. The histopathology of the cocoon membrane revealed the presence of dense fibrocollagenic tissue lined with mesothelium, along with a mixed cellular in fi ltrate, without any evidence of tuberculosis.
DISCUSSION
Since its fi rst description in 1907 by Owtschinnikow, the abdominal cocoon has remained an uncommon cause of intestinal obstruction in which bowel loops of variable extent are encased within a fibrous sac. Although a 'secondary' form of this disease has been well reported to arise in association with a variety of clinical situations such as practolol intake, chronic ambulatory peritoneal dialysis, ventriculo-peritoneal shunts, tuberculosis, etc., the etiology of the classical form of the disease is still not clear. This is typically seen in young, adolescent females from subtropical countries. In such 'primary' cases, it has been hypothesized that the encasing membrane or cocoon arises either as a result of subclinical peritoneal in fl ammation, immunological reaction to viral infections, or infections of the genital organs, or even, retrograde menstruation; however, as of now, there is no conclusive evidence to favor any of these theories, especially since more and more reports are coming out of the disease in older patients and even in males.[1–5]Our patient, too, adds to the growing list of idiopathic abdominal cocoon being seen in male patients, adding further to the questionability of the above mentioned hypotheses. We feel that the disease arises as a peritoneal reaction secondary to an exaggerated immune response to some yet, unidenti fi ed stimulus.
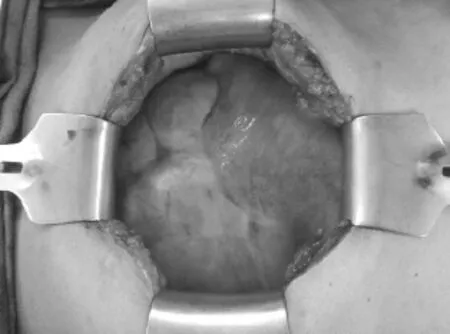
Figure 2. Photograph showing the cocoon encasing the bowel loops at the time of laparotomy.
Patients with abdominal cocoon present with signs and symptoms of intestinal obstruction that may be recurrent, and amenable to conservative management. A few radiological features that are suggestive of the disease have been described on ultrasonography (a thick-walled mass containing bowel loops, loculated ascites and fibrous adhesions), small bowel series (clumped together ileal loops showing a cauli fl ower-like appearance on sequential films) and CT scans (central clumping of small bowel loops, encasement by a soft tissue-density mantle, bowel wall thickening, localized fluid collections, etc.), but the condition is more commonly diagnosed during surgery when the membrane encased bowel loops are seen.[2,3,5]The cocoon usually involves varying parts of the small intestine, but can extend on to cover the colon, stomach, liver, and even spleen (as in our patient). Simply cutting through this membrane and releasing the contained bowel loops is curative in the large majority of patients with a primary cocoon, but at times,[2,4]extensive adhesiolysis and resection of the bowel may also be needed.[1]
Biopsy from the cocoon wall usually shows dense fibrocollagenic tissue along with a mixed inflammatory infiltrate, but is important in ruling out other causes such as tuberculosis.[1,4]Although we have encountered tuberculosis as a cause of abdominal cocoon previously,[4]this patient did not have any evidence of tuberculosis, thus clinching the diagnosis of an idiopathic abdominal cocoon.
Funding:None.
Ethical approval:Not applicable.
Conflicts of interest:The authors have no competing interests relevant to the present study.
Contributors:Jayant M proposed the idea, and Kaushik R wrote the paper. Both the authors contributed to editing the final manuscript for content and style.
REFERENCES
1 Rastogi R. Abdominal cocoon secondary to tuberculosis. Saudi J Gastroenterol 2008; 14: 139–141.
2 Xu P, Chen LH, Li YM. Idiopathic sclerosing encapsulating peritonitis (or abdominal cocoon): A report of 5 cases.World J Gastroenterol 2007; 13: 3649–3651.
3 Gupta S, Shirahatti RG, Joshi A. CT findings of an abdominal cocoon. Am J Roentgenol 2004; 183: 1658–1660.
4 Kaushik R, Punia R, Mohan H, Attri AK. Tuberculous abdominal cocoon - a report of 6 cases and review of the Literature. World J Emerg Surg 2006; 1: 18.
5 Wig JD, Gupta SK. Computed tomography in abdominal cocoon. J Clin Gastroenterol 1998; 27: 259–260.
Received November 20, 2013
Accepted after revision May 19, 2014
World J Emerg Med 2014;5(3):234–236
10.5847/ wjem.j.issn.1920–8642.2014.03.014
 World journal of emergency medicine2014年3期
World journal of emergency medicine2014年3期
- World journal of emergency medicine的其它文章
- Cardiac arrest: a case-based review
- Life-threatening complications of ascariasis in trauma patients: a review of the literature
- Instructions for Authors
- Effects of aspirin on the expression of nuclear factor-κB in a rat model of acute pulmonary embolism
- Attitudes towards child restrains and seat belts usage in the learned population of Karachi, Pakistan
- Hydrocolloid dressing in preventing nasal trauma secondary to nasal continuous positive airway pressure in preterm infants
