A case report of acute pulmonary vein stenosis
Xin-Yan Huang, Yu-Kun Kuang, Jian-Qiang Huang, Yu-Biao Guo
The Division of Pulmonary and Critical Care Medicine, The First Affiliated Hospital of Sun Yat-sen University, Guangzhou, China
1. Introduction
Hemoptysis refers to the bleeding of throat or any part of the respiratory system below the throat, and blood was discharged through the mouth. Although the amount of hemoptysis could be small or large, it often suggests important organic diseases.In China, common causes of hemoptysis include tuberculosis,bronchiectasis, lung cancer, and pulmonary infections [1]. In recent years, with the deepening of understanding of disease and the popularization of knowledge, hemoptysis, as a common emergency symptom, will also cause many doctors to consider the possibility of pulmonary embolism, especially in the emergency department.Since hemoptysis, chest pain, and dyspnea are typical tiads of pulmonary embolism, doctors often need to rule out the possibility of pulmonary embolism first for patients with hemoptysis and chest pain who seek treatment in emergency department, but there are also rare cases showing similar symptoms. This article reports a case of “hemoptysis and chest pain” as initial symptoms. The patient was transferred to a number of hospitals for medical treatment, but has not been correctly diagnosed until 7 months later. This article aims to improve clinician’s ability to make differential diagnosis of hemoptysis.
2. Case report
The patient was a 46-year-old male and Han nationality. The patient was admitted to our hospital on July 5, 2015 due to recurrent coughing, coughing phlegm and chest pain for more than 7 months.More than seven months before admission, the patient developed coughing, coughing of small amount of sticky, yellow phlegm,accompanied by hemoptysis, left chest pain, and the chest pain could be relived after a break. No breathing difficulties, fever or palpitations was detected. He initially went to a local hospital for emergency treatment, and the diagnosis was “considering pulmonary embolism”, chest enhanced CT examination showed upper left lung pneumonia, but no clear pulmonary thromboembolism was revealed, then he was given anti-infective treatments.
After the treatment, the patient’s symptoms did not improve significantly. Serial chest CT scans suggested left upper lung exudation shadow. The patients was given anti-infective therapy including ceftriaxone, cefoperazone/tazobactam, and moxifloxacin in local and Guangzhou hospitals successively. During these hospital visits, the patient also underwent T-SPOT test, TB-DNA quantification, cytomegalovirus detection, and sputum culture. No abnormalities were observed. Transbronchoscopic lung biopsy was performed and pathology showed that “mild interstitial fibrous hyperplasia, and the tissue cells in some alveolar cavity were clustered. No neoplastic lesions was found, and possibility of fungal or tuberculosis infection was considered.” In an external hospital he was given diagnostic anti-tuberculosis treatment (HRZE) for one month, but the patient’s symptoms did not significantly improve after the treatment. There was still intermittent coughing with bloody sputum. About 5 months before hospitalization, hemoptysis and hemorrhoids were more prevalent than before, and CT scans suggested a new lesion in the left lung. Further PET/CT showed that there was no metabolic shadow of malignant tumors and the possibility of inflammatory lesions was high. The patient underwent percutaneous lung puncture. The pathology showed “consideration of an inflammatory lesion.” The rheumatic immunologic markers were negative. He was suspected of being vasculitis and was treated with oral prednisone (20 mgbid.) and the dosage was gradually tapered. However, the patient still had bloody sputum accompanied with a small amount of hemoptysis. For further treatment, the patient was admitted to our hospital.
The patient had previous history of hypertension, atrial fibrillation.He had a history of tuberculosis but had been cured. Three years ago, he underwent circumferential pulmonary vein isolation through bilateral pulmonary vein antrum approach. He had history of smoking for more than 20 years, 1 pack/day, but had quitted smoking for more than half a year. Personal history, marriage, childbearing history, and family history are not special.
Admission physical examination showed wet rale in the left upper lung, no other special signs were found. After admission, blood routine showed: WBC 7.53×109/L, NEU% 55.8%, EOS% 0.4%,Hb 124g/L, PLT 162×109/L. There were no obvious abnormalities in biochemistry tests, liver and kidney function. PCT was 0.03 ng/mL and ESR 29 mm/h. G test, cryptococcal antigen, Aspergillus antigen tests were all negative. PPD skin test results were negative,rheumatism, SLE 5 items, ANCA combination detection, antiphospholipid syndrome combination detection reveal no abnomality.Lung tumor markers, serum immunoelectrophoresis was normal too.Pulmonary function tests showed that lung diffusion function was slightly decreased but the ventilation function was normal, and the histamine challenge test was negative. Cardiac echocardiography showed that increased size of both left and right atrium, mitral insufficiency (mild), the left ventricular systolic function was normal but diastolic function was reduced. Chest CT performed on 9 July 2015 showed multiple nodules, cluster-like and patchy shadows in the left upper lung with blurred border. No calcification or obvious cavities were seen. No obvious enhancement after enhanced scan.There was a slight thickening and adhesion of the adjacent pleura.The bilateral lung fields were scattered in small patchy dark shadows. Multiple lymph nodes were seen behind the vena cava and bilateral hilar, the maximum diameter of the lymph node was about 15 mm (Figure 1). In our hospital, bronchoalveolar lavage fluid culture, smears, acid-fast bacilli, and Aspergillus antigens were found to be normal. Brushes tests reveal hemosiderin cells.Prednisone was stopped gradually, and moxifloxacin, fluconazole,and voriconazole were applied for antifungal treatment.
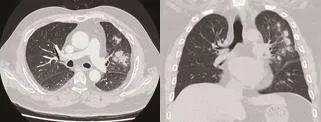
Figure 1. Chest CT showed multiple shadow in both lungs during admission.As the patient’s diagnosis was not clear, CT-guided lung biopsy was performed on 29 July 2015 which revealed necrotic tissues, local alveolar Type II epithelial hyperplasia, but no clear specific pathogen infection was found. At the same time, chest CT was performed on 4 August 2015. Compared with the detection results on 29 July 2015, the lesion size was slightly larger, and the density was thicker indicating possibility of fungal infection. Palpitations occurred during hospitalization, with a heart rate of 160 beats per minute,irregularities, and varying degrees of abnormal heart sounds. The ECG showed atrial fibrillation and was ameliorated after treatment with Amiodaronum.
The diagnosis of this patient was unclear. We invited experts from Cardiology Department and Radiology Department for consultant.Chest CT data was reviewed and pulmonary venous stenosis was considered (Figure 2) which is a postoperative complication of circumferential pulmonary vein isolation. Considering it is unable to place stents for stenting, the patient underwent left upper lobe resection on a surgically-assisted thoracoscopic surgery on 8 August,2015. Surgical pathology revealed multifocal coagulative necrosis in the lung, peripheral fibrovascular hyperplasia accompanied with lymphocytes, and plasma cell infiltration. In the nodule, a large number of hemosiderin cells were seen in the surrounding alveolar cavities, the alveolar septum was widened, and fibroplasia was accompanied by inflammatory cell infiltration, which were consistent with chronic inflammatory changes. No malignant characteristics were observed (Figure 3). Follow-up showed no relapse of coughing,bloody sputum or chest pain. But chest radiograph detection showed parcel liquid pneumothorax of the left upper lung (Figure 4).
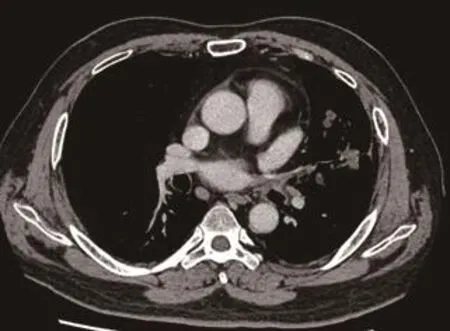
Figure 2. Pulmonary venous stenosis was= considered.
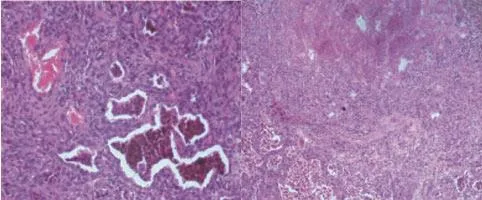
Figure 3. Surgical pathology.

Figure 4. Follow up chest radiograph image.
3. Discussion
This is a rare and difficult case, in which the patient starts with symptoms of cough, hemoptysis, and chest pain. It is often initially diagnosed in emergency department, respiratory department, and it is also easily misdiagnosed as pulmonary embolism. This case was repeatedly hospitalized three times in three different grade III A hospitals before attending our hospital and has been treated with antibacterial, anti-fungal, anti-tuberculosis and anti-rheumatism. Thus,he has been misdiagnosed for up to 7 months. The reason why this case was misdiagnosed was that the emergency department and the respiratory doctor had insufficient knowledge of the disease because of special disciplines, and they had insufficient understanding of the postoperative complications of the treatment of atrial fibrillation by circumferential pulmonary vein isolation. Therefore, they failed to make a correct diagnosis in time. In fact, there are not many physicians who understand that pulmonary venous stenosis is a complication of circumferential pulmonary vein isolation. Therefore,we reported this case with the aim of attracting the attention of more doctors.
Pulmonary venous stenosis is caused by a variety of factors that cause pulmonary venous stenosis, resulting in obstruction of pulmonary venous return and then producing a series of clinical manifestations. According to the cause of the disease, it can be divided into two kinds: congenital and acquired[2]. Acquired pulmonary venous stenosis is more commonly seen in adults, and it is common in the complications of drainage and correction of complete pulmonary venous malformation, but there are also reports in the literature indicating that it is related to fibrosus mediastinal,thoracic radiotherapy, malignant tumors, sarcoidosis, etc[3]. In recent years, with the increase of radiofrequency ablation for atrial fibrillation, literatures of this disease as a complication are also increasing. Reported incidence of pulmonary vein stenosis after radiofrequency catheter ablation of atrial fibrillation was 3.1%[4]and clinical manifestations are related to the degree of pulmonary vein stenosis and the number of involved blood vessels. Patients with mild or one-vein venous stenosis are often asymptomatic and about 60% of the patients are reported in the literature[4]. Patients with multiple vein involvement or severe stenosis often present with dyspnea, pleural inflammatory chest pain, cough, hemoptysis,recurrent pulmonary infections, etc, and they have hemoptysis with a small amount of hemoptysis or sputum with blood, but there are also reports of major hemoptysis in the literature[5]. The disease is often misdiagnosed as pulmonary embolism, pneumonia, lung cancer and other diseases. There are also reports of patients with pulmonary infarction as the major manifestation, and was misdiagnosed as organizing pneumonia.
Imaging diagnostic methods for pulmonary vein stenosis include echocardiography, enhanced CT, magnetic resonance imaging, and angiography[6], in which angiography can be the most effective and detailed observation of pulmonary veins. However, in recent years, the use of thin-slice high-resolution CT can reconstruct the left atrium posterior wall and each pulmonary vein and its proximal branches, can observe the diameter of each pulmonary vein opening through different angles and also can assess the extent and location of pulmonary vein stenosis. Thus, it is considered as an important noninvasive imaging method for diagnosing this disease. Therefore,invasive angiography is not routinely performed. However, it is worth noting that in the CT imaging diagnosis of the disease,the provision of clinical history is very important. After confirm diagnosis of this case, the patient‘s chest CT were reviewed and the changes of pulmonary vein stenosis were seen. However, due to the lack of medical history, radiologists may miss the diagnosis because they have not undergone revascularization.
In our case, the left upper lobe was finally resectioned, and postoperative lung pathological changes suggested multifocal coagulative necrosis and inflammatory cell infiltration, and hemosiderin cells were seen in the alveoli. The above pathological changes can easily be misdiagnosed as common inflammation,tuberculosis or vasculitis in small specimen biopsies. However, The pulmonary pathological changes of this disease are relatively rare in domestic and foreign literature reports[7]. This case can provide reference for the identification of future pathology.
As atrial fibrillation is often followed by a cardiologist after radiofrequency ablation, the complications of the disease can be detected in time. Only a few patients are first diagnosed in the emergency department and have respiratory complications.This patient, as a rare case, many things are worth learning in the diagnosis and treatment, especially for clinicians to pay attention,this case suggesting that the importance of the combination of basic medicine and multidisciplinary medicine is very important in modern medicine.
Conflict of interest statement
We declare that we have no conflict of interest.
[1] Zhong NS, Liu YN.Respiratory diseases. 2nd ed. Beijing: People’s Medical Publishing House;2012,p.72-74.
[2] Latson LA, Prieto LR. Congenital and acquired pulmonary vein stenosis.Circulation2007;115(1):103-108.
[3] den Bakker MA, Thomeer M, Maat AP, Groeninx van Zoelen CE. Lifethrentening hemoptysis caused by chronic idiopathic pulmonary hilar fibrosis with unilateral pulmonary vein occlusion.Ann Diagn Pathol2005;9(6):319-22.
[4] Packer DL, Kowal RC, Wheelan KR, Irwin JM, Champagne J, Guerra PG, et al. Cryoballoon ablation of pulmonary veins for paroxysmal atrial fibrillation: first results of the North American Arctic Front (STOP AF)pivotal trial.J Am Coll Cardiol2013; 61: 1713-1723.
[5] Lee JY, Chon GR, Park JH, Kang BJ, Shim TS, Jo KW. Massive hemoptysis due to pulmonary vein stenosis following catheter ablation for atrial fibrillation.Respir Care2015;60(3):e52-e55.
[6] Saad EB, Rossillo A, Saad CP, Martin DO, Bhargava M, Erciyes D, et al.Pulmonary vein stenosis after radiofrequency ablation of atrial fibrillation:functional characterization, evolution, and influence of the ablation strategy.Circulation2003;108(25):3102-3107.
[7] Kwon MR, Lee HY, Cho JH, Um SW. Lung infarction due to pulmonary vein Stenosis after ablation therapy for atrial fibrillation misdiagnosed as organizing pneumonia: sequential changes on CT in two cases.Korean J Radiol2015;16(4):942-946.
 Journal of Acute Disease2018年1期
Journal of Acute Disease2018年1期
- Journal of Acute Disease的其它文章
- Acute intra-operative brain swelling managed effectively with emergency basal cisternostomy: A case report
- Diminazene aceturate modified nanocomposite for improved efficacy in acute trypanosome infection
- Role of first day levels and subsequent trends of serum proteins in acute burns
- Progress in the surgery of rectal cancer
- The laparoscopic approach in emergency surgery: A review of the literature
- Acute myocardial infarction and Yin Yang imbalance
