Childhood bullous pemphigoid with progressive muscular dystrophy:a case report
Yuan Ding,Jing-Zhan Zhang,Buwajieer Yakeya,Shi-Rong Yu,Fang Xiang,De-Zhi Zhang,Xiao-Jing Kang*
Department of Dermatology,People’s Hospital of Xinjiang Uygur Autonomous Region,Urumqi,Xinjiang 830001,China.
Introduction
Bullous pemphigoid(BP)is an acquired autoimmune disorder,which is clinically characterised by subepidermal blistering,eosinophilia,and severe itch,and it can be complicated by a variety of senile diseases,including neurological diseases.BP mostly attacks older people and is considered rare in children.BP patients were often comorbid with neurological diseases, including dementia, stroke, epilepsy,Parkinson’s disease,and multiple sclerosis has been demonstrated.
Progressive muscular dystrophy(PMD)is a hereditary skeletal muscle degenerative disease,and is the most common and serious neuromuscular disease in children,but the child with BP and PMD has never been described.Herein we reported a young case of teenage with both diseases.
Case report
The patient was a 17-year-old boy,who was admitted to the People’s Hospital of Xinjiang Uygur Autonomous Region for the chief complaint of blistersand erythema,with itching for 1 month and aggravation for 3 days.Initially,there were only a few erythema and blisters about the size of rice on his arms with mild itching.The lesions gradually increased and also appeared on the shanks.Therefore,he visited a community clinic for treatment.The specific diagnosis was unknown,and Eloson ointment was provided for external application,but the effect was unsatisfactory.Over the recent 3 days,remarkable edema,as well as bullae about the size of broad bean,was found on his shanks.Therefore,the patient was admitted to the People’s Hospital of Xinjiang Uygur Autonomous Region with the diagnosis of linear immunoglobulin A(IgA)bullous dermatosis.
The patient was diagnosed with progressive muscular dystrophy in 2009 with deletion of exon 50 in the dystrophin gene.He received cord venous blood stem cell transplantation twice and transvenous autologous bone marrow stem cell transplantation once.He also received four-extremity autologous bone marrow stem cell transplantation once and collection of bone marrow stem cells once after 4-day mobilization by filgrastim.At present,the patient is not taking any therapeutic medicine.His mother is a pathogenic gene carrier,and his parents are not close relatives.His father,sister,and younger brother were all teported to be normal.
A dermatological examination showed blisters and bullae with the size of rice grain to broad bean.These features were densely distributed on the face,trunk,limbs,hands,feet,and scrotum.Part blisters were arranged annularly.The extremities mainly presented with bullae accompanied by edema of both feet,and there were multiple targetoid erythemas scattered on the trunk(Figure 1A).Nikolsky’s sign was negative.
A physical examination showed scoliosis deformity,and the patient’s muscular strength was at gradeⅠ for the lower extremities and gradeⅢfor the upper extremities.Other systemic examinations did not show any remarkable abnormalities.A routine blood test showed the following:the white blood cell count was 9.46×109/L,red blood cell count was 4.75×1012/L,platelet count was 308×109/L,eosinophil count was 1.84×109/L,and the percentage of eosinophils was 19.5%.A biochemical panel test showed that the albumin level was 38 g/L and the creatine kinase level was 510 U/L.The erythrocyte sedimentation rate was 8 mm/h.Humoral immunity and autoantibodies were negative.BP180 was 200 Ru/ml.The blood IgE level was 345 U/L.An electrocardiogram and X-ray chest films were normal.Abdominal and urinary B-mode ultrasonography showed that the liver,gall bladder,pancreas,and spleen were free of abnormalities.
A histopathological examination showed subepidermal blisters with massive eosinophilic infiltration in the blister fluid(Figure 1B).Direct immunofluorescence(DIF)confirmed the presence of linear IgG and complement 3(C3)along the basement membrane(Figure 1Cand1D),and IgA was weakly positive(Figure 1E),but IgM was negative(Figure 1F).This was consistent with pathological changes of BP.The patient was diagnosed with childhood BP with progressive muscular dystrophy.
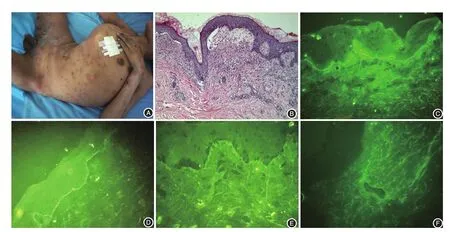
Figure 1 Bullous pemphigoid lesions and histopathology of the patient.A:multiple targetoid erythemas and blisters on the patient’s trunk with scoliosis deformity.B:a subepidermal blister with eosinophilic infiltration(Haematoxylin and Eosin,×40).C:Linear IgG depositions along the basement membrane zone(Direct immunofluorescence,×200).D:Linear C3 depositions along the basement membrane zone(Direct immunofluorescence,×200).E:IgA is weakly positive(Direct immunofluorescence,×200).F:IgM is negative(Direct immunofluorescence,×200).
Discussion
BP is characterized by linear sedimentation of IgG and/or C3 at the basal membrane zone.There are autoantibodies against BP230(BP antigen 1)and BP180(BPantigen 2)in serum.Childhood bullous pemphigoid(CBP)is a less common subtype of BP compared with adult BP,and its prognosis is relatively satisfactory[1].Gajic-Veljicet al.[2]analyzed the clinical features of CBP in six children aged from 2 to 17 years.The average age was 10,and the rate of oral mucosa involvement was higher than that of adults BP.Generally,the rate of extremity involvement was lower in children BP than that of infants younger than 1 year old with BP.
In our 17-year-old patient,his oral mucosa was not involved,and his initial manifestation was remarkable blisters and erythema on the extremities.The patient manifested with typical lesions,as well as annular blisters and bullae,which were consistent with pleomorphic lesions caused by pemphigus.However,he also developed annularly arranged blisters,which were difficult to be differentiated from childhood linear IgA bullous dermatosis.Although BP180 was positive in serum,a diagnosis of BP was unable to be made,because BP180 is also a key antigen in childhood linear IgA bullous dermatosis[3].
Direct immunofluorescence results slightly differ for BP patients with different ages.Schwieger-Brielet al.[4]analyzed the features of 81 infants with BP.Compared with adult patients,the BP180 positive rate was relatively higher in children,and linear IgG and/or C3 sediment(s)were found at the basal membrane zone.Furthermore,childhood BP could present with mild IgA or IgM sediment(s)in addition to linear IgG and(or)C3 sediment(s).In our case,the patient manifested with IgG and C3 sediment(s)as well as mild IgA sediment,which is consistent with the immunofluorescence mode of childhood BP.Furthermore,a histopathological examination showed typical subepidermal blisters with massive eosinophilic infiltration in the blister fluid,which is consistent with histopathological features of BP.
The patient’s blood IgE level was 345 U/L with a remarkably elevated eosinophil level,and it was consistent with clinical features of BP.A previous research[5]has shown that total serum IgE levels in patients with BP are positively correlated with the antibasal membrane zone IgG antibody level and disease activity.In addition,they found that the lesions that cause elevated levels of total serum IgE were urticaria and erythema,instead of blister and erosion.Elevation of eosinophil,which is an important perivascular marker in early onset of BP,is related to the disease severity.When the patient was discharged,the blood IgE and eosinophil levels returned to normal.
The final diagnosis is BP based on histopathological examinations and direct immunofluorescence results.The patient was intravenously administered 40 mg of methylprednisolone.Two weeks later,the skin lesions completely receded.The outcome of treatment further confirmed the diagnosis of BP,because childhood linear IgA bullous dermatosis is not sensitive to hormonal therapy,and the preferred treatment is dapsone.
In our case,the patient also had progressive muscular dystrophy.A retrospective research domestically and overseas has shown that BP patients were often comorbid with neurological diseases, such as cerebrovascular diseases(cerebral thrombosis and cerebral hemorrhage),epilepsy,vascular dementia,Alzheimer’s disease,Parkinson’s disease,tremors,multiple sclerosis,and hemiplegia.Previous studies have shown that a long-term bedridden state and pressure sore caused by neurological diseases are closely correlated with the occurrence of BP[6].
Liet al.[7]concluded that,for BP patients comorbid with neurological diseases,neurological diseases usually occur firstly and then BP comes.The interval between these two diseases can be from several months to several years.The mechanisms of BP comorbid with neurological diseases have been investigated.BP 180 was confirmed to be expressed in human brain neurons,and its mainly targets include somatic cells of human neurons and proximal axon brain tissue[8].Neurological lesions cause exposure of neurological antigen subtypes to the immune system,and may result in cross-reactivity on skin subtypes of BP 180 by immune system,leading to the appearance of bullous pemphigoid[9].
Progressive muscular dystrophy(PMD)is a hereditary skeletal muscle degenerative disease,and is the most common and serious neuromuscular disease in children.PMD is caused by mutations in theDMDgene encoding a protein called dystrophin.TheDMDgene includes 79 exons,and the mutation occurs mainly between exons 45-54 leading to loss of dystrophin expression,consequently resulting in destruction of the integrity of muscle fiber membrane in patients with DMD.When the muscle is pulled and contracted,it is easily damaged or even degenerated and necrotic.Dystrophin is expressed not only in skeletal muscle but also extensively in hippocampal pyramidal neurons,pyramidal neurons in the neocortex,amygdaloid nuclei,and cerebellar purkinje cell postsynaptic membranes.Therefore,dystrophin protein has great biological significance in maintaining the normal physiological status of central nervous system[10].Our patient received gene analysis to confirm the diagnosis of PMD,and if the connection exists between PMD and BP needs to be further invesitigated in this case.
In summary,the coexistence of childhood BP,and DMD has never been reported,and our case riches the knowledge of BP.Although the precise reason why our case exhibited these two diseases is not completely understood,we speculate that these conditions may be associated with epitope spreading,and it needs further genetic studies to confirm.
- 國際皮膚性病學(xué)雜志的其它文章
- Paraneoplastic pemphigus comorbid with cardiac cancer and duodenal gastrointestinal stromal tumors:a rare case report
- Reactive perforating collagenosis
- Sun?protection knowledge and strategies of Chinese dermatologists:a nation?wide,questionnaire?based survey
- Initial presentation of acute myeloid leukemia in a patient with cutaneous myeloid sarcoma
- Persistent papules with adult?onset Still’s disease:a case report
- Primary vulvar melanoma in a 27?year?old pregnant woman:a case report and literature review