Changes in SchIemm’s canaI,trabecuIar meshwork,and reIevant parameters in the earIy stage after SMILE of myopia patients
INTRODUCTION
At the beginning of this century,the femtosecond laser was introduced in China,which made corneal laser surgery progress into a knifeless era.The effectiveness,safety,stability,and predictability of the treatment of low,middle,and high myopia have been reported.Small incision lenticule extraction (SMILE) has entered the era of “minimally invasive”corneal laser surgery because of its minimal incision design and lens separation method.There are a growing number of reports about the effectiveness of SMILE.The researchmainly focuses on the advantages in visual quality,corneal biomechanical stability,and the reduction of dry eyes after SMILE.There are few reports on the changes in the anterior chamber,especially those in Schlemm's canal (SC) and the trabecular meshwork (TM) as well as related parameters in China and the other countries.SC and TM are the important components of the anterior chamber angle and the main pathway for aqueous outflow.Changes in the SC and TM are also related to changes in intraocular pressure (IOP).It is known that the use of suction is an important part of SMILE surgery.While suction is applied,the IOP of the anterior chamber rises sharply,but whether this has some influence on the anterior chamber angle is unknown.Furthermore,the central corneal thickness (CCT),the corneal curvature,and corneal biomechanics change after SMILE may affect IOP measurements.Therefore,real changes in IOP are easily concealed,especially in some patients who develop glaucoma after SMILE.Previous studies have suggested that glaucoma patients have narrower SC than healthy individuals.Reduced SC size may be associated with elevated IOP because the dimension of SC is closely related to TM outflow.This study aimed to analyze changes in real IOP after SMILE by observing the changes in the SC and TM,to detect and diagnose those patients with glaucoma after SMILE earlier.In addition,it is known that the occurrence of primary open angle glaucoma (POAG) is often closely related to high myopia.Our previous studies also revealed some differences between the SC and TM in patients with high myopia and those with low and moderate myopia.We wanted to observe the changes in the SC and TM in SMILE patients with high myopia to see if they are different in those patients with low and moderate myopia,in order to better understand the individual differences of SC and TM in patients with high myopia.
SUBJECTS AND METHODS
The research was approved by the Institutional Review Board and followed the tenets of the Declaration of Helsinki.All subjects signed informed consent.
The family had just moved to Rhode Island, and the young woman was feeling a little melancholy1() on that Sunday in May. After all, it was Mother s Day -- and 800 miles separated her from her parents in Ohio.
From December 2018 to January 2019,patients aged between 18 and 40y who underwent SMILE surgery at EyeGood Ophthalmological Hospital of Wuhan were enrolled.A total of 58 eyes from 30 patients (8 males and 22 females)who underwent SMILE were divided into group A:a low and moderate myopia group (≥-6 D),32 eyes,spherical correction-4.4±1.0 D,cylinder correction -0.70±0.5 D;group B:a high myopia group (<-6 D),26 eyes,spherical correction -6.5±0.7 D,cylinder correction -0.70±0.5 D.These groups are according to equivalent spherical lenses (spherical lenses+1/2 columnar lenses).All patients were completed routine preoperative examinations,preoperative corneal thickness ≥480 μm,refraction ≤12 D,and predicted residual corneal stromal bed≥280 μm were included,excluding contraindications.
One day the Prince went out hunting, and going in pursuit of a wild boar he soon lost the other huntsmen, and found himself quite alone in the middle of a dark wood
The TM diameter,cross-sectional area,TM width and thickness of the temporal SC in groups A and B were observed pre-and postoperatively at 1d (post-1d),1wk (post-1wk),and 1mo (post-1mo).The corneal curvature (K1,K2),anterior chamber depth (ACD),average anterior chamber angle (ACA),anterior chamber volume (ACV),and Ehlers and Shah formula-corrected IOP were recorded in Pentacam measurements before and after surgery.The changes in accommodation amplitude (AMP) before and after surgery were measured.The changes in the SC and TM after surgery and the related factors were analyzed.
The horizontal diameter and cross-sectional area of the temporal SC,and the width and thickness of the TM,were observed by CIRRUS HD-OCT5000 (ZEISS) anterior segment scanning (with a corneal lens added).Studies have shown that the diameter and cross-sectional area of the SC on the nasal and temporal side are the largest.Each measurement should fix the head eye position,such that the eye position of the same patient is consistent with each examination.The position of each eye was measured three times at the 9 o'clock (right eye) or 3 o'clock (left eye) on the temporal side.The highest possible image quality was obtained.All patients were examined by the same operator.
He immediately summoned all the best doctors in the country, and they came with all their prescriptions14 and their medicine bottles, but next day the princess was stiff and cold in death
Pentacam anterior segment analysis system (Germany OCULUS company) was used to examine the anterior segment.The examinations were performed in a dark room,and the images with QS as OK were selected.Each eye was measured twice,and the average value of the central ACD,average ACA,and ACV were recorded.
Does refractive surgery affect the anterior segment,especially the adjacent anterior chamber angle? Will it affect the relevant factors of the outflow pathway of the aqueous humor? Per our knowledge,there are few reports about the anterior and posterior segment changes after refractive surgery at home and abroad,and there is no unified conclusion.There have been some controversies.According to the results of one study,we analyzed the changes in the SC and TM related to the following factors and discussed the effects of the changes in SC and TM on IOP after SMILE.
This study aimed to observe the changes in the SC and TM after SMILE.The SC is an aqueous outflow pathway around the corner of the anterior chamber.High frequency ultrasound biomicroscopy (UBM) and OCT are used to observe the size and diameter of SC.Both techniques can measure the diameter of the SC on images.OCT is widely used in related research because of its simple operation,non-invasiveness,good repeatability,and high rate of identification.For observation of the SC,sweep source OCT (SS-OCT) and frequency domain OCT (FD-OCT) have been mainly used in similar studies.In this study,the SC and TM were observed by CIRRUS HD-OCT5000 (Zeiss Company,Germany).This is an optical coherence tomography angiography (OCTA) scanner with its own vascular imaging and panoramic anterior segment module.Clinically,it is mainly used for the diagnosis of retinal diseases and macular diseases.Its special angiography and analysis function is relatively new in the field.In the fundus diseases,CIRRUS HD-OCT is considered to be irreplaceable by other devices.The main advantage of OCTA in the anterior segment is that it can quickly acquire images using non-contact technology.Some researchers use OCTA to measure corneal thickness.Compared with other devices,OCTA also has a high reference value.At present,there is no relevant literature to report its research on the SC.Because this study was carried out using the same equipment at different times,and our comparison of the related data on the SC and TM in low,moderate myopia and high myopia groups shows the same trend reported in other related studies.
Rebekah was only 32, admitted for chemotherapy() after breast-cancer surgery, When I entered her room it took me a moment to spot her amid the bouncing forms of three giggling5 little girls.
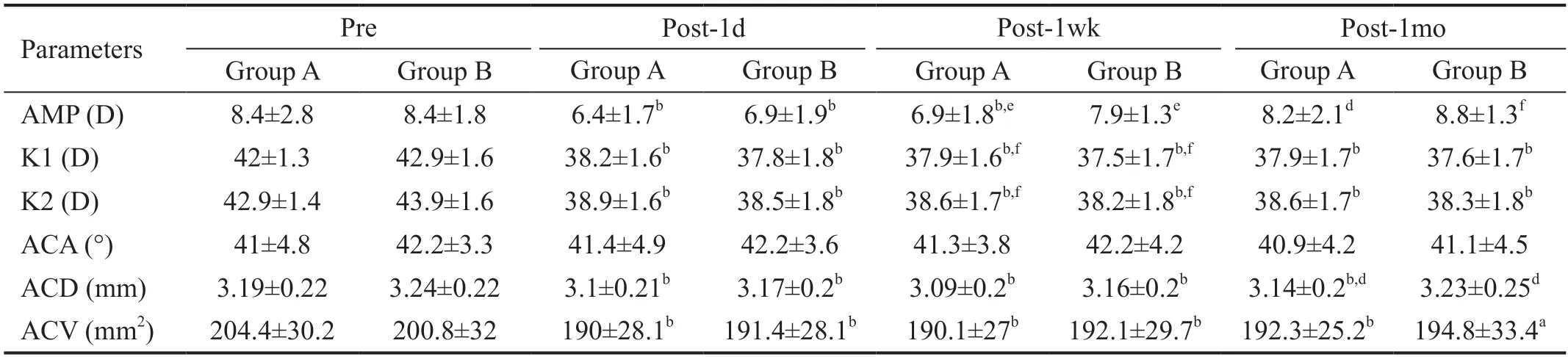
Through this study,found that the AMP of SMILE in both groups decreased at first day,then increased gradually postoperatively.By 1mo after SMILE,the AMP of SMILE had returned to preoperative levels.AMP is the maximum accommodation force that the human eye can produce.When people need more than half of the possible AMP,visual fatigue symptoms will occur.In the early stage after refractive surgery,most of the patients are in the mild hyperopia state.Because of the change of the refractive state and the decrease in AMP,the accommodation force needed for myopia is increased,and the corresponding ciliary muscle contraction is obvious,which leads to a series of changes.
SPSS 23.0 software was used to analyze the data.The measurement data were expressed as mean±standard deviation (SD).Paired sample-test was used to compare the data of group A and group B before and after surgery.Independent sample-test was used to compare the data of group A and group B.Pearson correlation was used to analyze the changes in the SC cross-sectional area and its related factors.<0.05 was considered statistically significant.
RESULTS
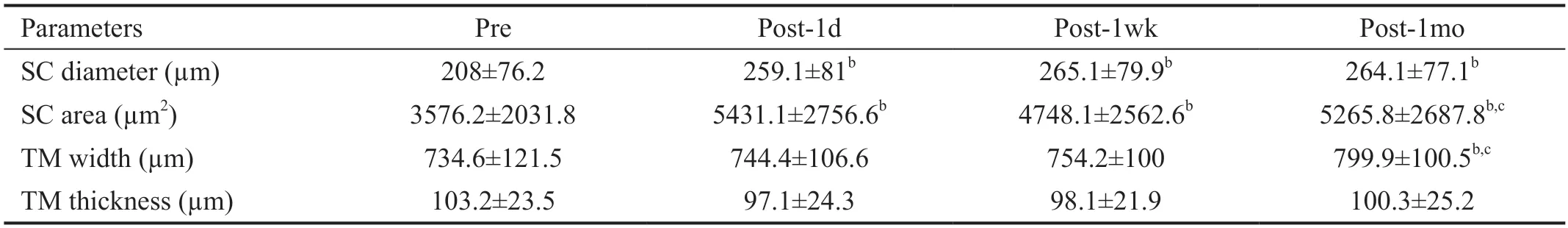
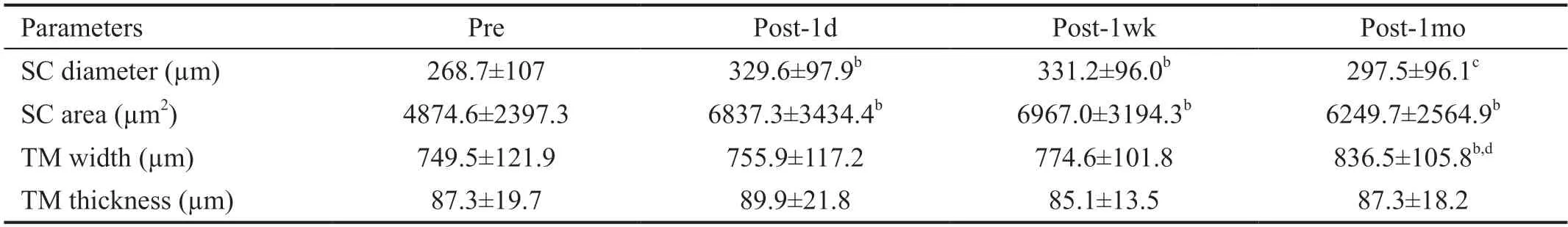
The diameter of the SC was significantly increased postoperatively (<0.01),and there were no statistical differences between the different time points after surgery(>0.05) in group A (Table 1).The SC area was significantly increased postoperatively (<0.01).The width of the TM was only significantly increased at the post-1mo (<0.01).The thicknesses of the TM were not statistically significant differences between any of the time points (>0.05;Table 1).The diameter of the SC was significantly increased at post-1d and post-1mo (<0.01),and there was no statistically significant difference between the pre-and post-1mo (>0.05) in group B (Table 2).The area of SC was significantly increased after surgery (<0.01).There was no significant difference between the different time points after surgery (>0.05).The width of the TM was only significantly increased at the post-1mo (<0.01).The thickness of the TM was not statistically significant difference between any of the time points (>0.05;(Table 2).
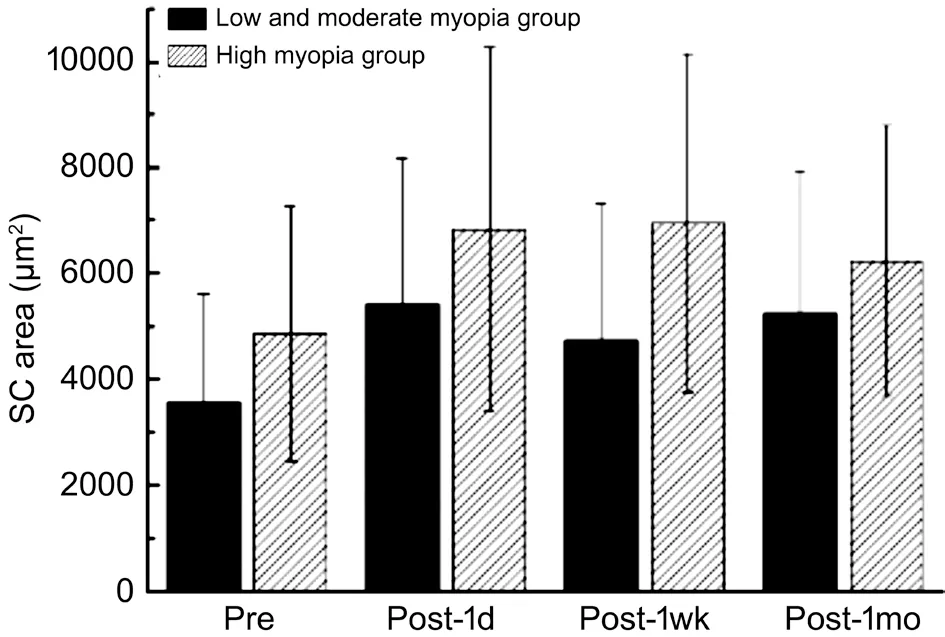
There was no significant difference between the two groups pre-and postoperatively (>0.05).Only post-1wk to post-1mo,the change in the SC area in the low and moderate myopia group was significantly different from the high myopia group(<0.05).The SC area in the low and moderate myopia group showed an increasing trend,while that of the high myopia group showed a decreasing trend (Figure 2).

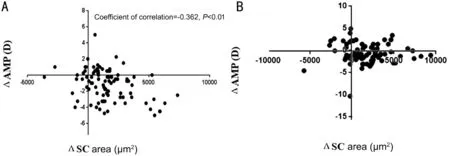
There was a weak negative correlation between the change of the SC area (ΔSC area) and that in AMP (ΔAMP) in group A (=-0.362,<0.01),but no correlation between the ΔSC area and the ΔAMP in group B (Figure 3).The changes in SC area showed no correlation with the change in IOP,corneal curvature,and the anterior chamber parameters (ACD,ACV,and ACA).
36. Tis Heaven s own child,/The tempest wild, : The children are trying to make the woman believe the wind is causing the noise outside her house. I prefer Jack Zipes translation of the children s reply for clarity:
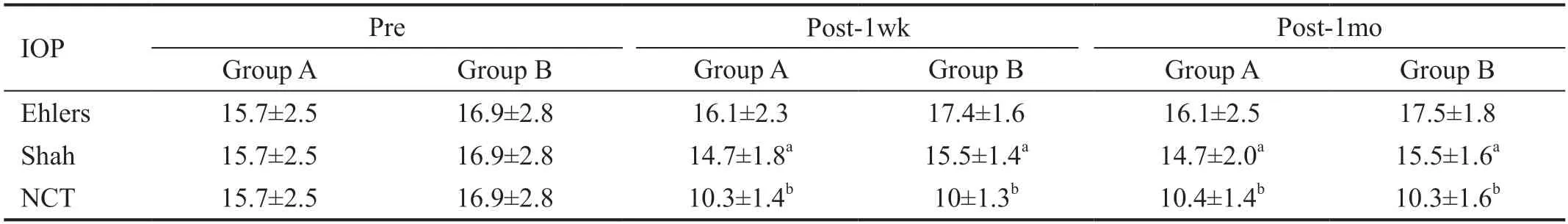
The corrected IOP Shah formula of the two groups indicated that the IOP post-1wk and post-1mo was significantly lower than that of the preoperative (<0.05).Ehlers formulacorrected IOP showed that there was no significant difference in IOP between the two groups at the post-1wk and post-1mo(Table 3).
Second,ciliary muscle contraction,suspension ligament relaxation,lens thickness increase,lens diameter decrease,and anterior part obvious protrusion result in a shallow ACD.This study found that the ACD after surgery in the low and moderate myopia group was less than that before surgery.The changes in ACD in the high myopia group was the same as that seen in the low and moderate myopia group,only 1mo after surgery,the ACD was close to that before surgery.In addition,the ACV of both groups showed that all time points after surgery were smaller than those before surgery,and there was no significant difference between the changes after and before surgery,suggesting that the ACV became smaller,and the ACA did not change significantly in the early stage after SMILE.This study also verifies that the change in ACD has a weak positive correlation with the change in ACV and TM width.However,we do not exclude other factors that can affect ACD,such as changes in the posterior corneal surface and biomechanical changes.In previous reports,changes in the posterior corneal surface after excimer laserkeratomileusis (LASIK) surgery have been controversial.Cairnsfound that after LASIK,the posterior corneal surface protrusion and ACD became shallower.It is believed that the anterior process of the lens after LASIK is larger than posterior corneal surface protrusion.Dupps and Robertsbelieve that the corneal posterior surface protrusion is because the biomechanical strength of the posterior stroma lower than that of the anterior stroma.Yuused a Pentacam device to measure the posterior elevation in their latest study.Orbsan may misjudge that the posterior corneal surface is too high after SMILE.It was found that the ACD became shallow after SMILE,and the posterior corneal surface became flat and retracted.This study shows that no matter how the posterior corneal surface changes,the change of the accommodation after surgery is certainly one of the reasons for the decrease in ACD,and it also causes the expansion of the SC lumen.
DISCUSSION
The AMP was the maximum accommodation of eyes.The negative lens method was used to measure AMP,and both the left and right eyes were measured in the following manner:the non-test eye was covered,the test eye was corrected to achieve the best visual acuity,and the visual target was fixed (the last line of the best visual acuity in close range) and kept clear.Negative lenses were gradually added before the test,in increments of -0.25 D,until the point at which the subject's vision was continuously blurred.The absolute value of the sum of the degrees of the negative lens added together with the reciprocal of the distance between the eye and the lens (.,2.5 D),is the AMP of the patient.All patients' measurements were performed by an optometer,twice each time,and the average value was taken for data analysis.
The Ehlers and Shah formulas in Pentacam were selected.The corrected IOP of Ehlers and Shah formulas after surgery was obtained by using the results from non-contact tonometer(NCT) measurements (average measurements were taken three times per eye) and the changes in IOP displayed in Pentacam.
In recent years,several studies on POAG focus on the SC.Although the pathogenesis of POAG has not been fully revealed,it can be clear that the SC is an important factor in the pathogenesis of POAG.Some studies have reported that the area of the SC in POAG patients is significantly smaller than that of healthy people,and the number of SC lumen is less than that of healthy people.Therefore,the aqueous outflow in POAG patients is blocked and the IOP is increased.The size of the SC is also related to factors such as age and diopter.The diameter and area of SC decreases with age.The diameter and area of the SC in individuals with high myopia are larger than in those with low and moderate myopia.Some studies have also found that the SC of healthy people will expand significantly after exercise.We speculate that the change in SC size is also related to the regulation of the autonomic nerve.Xinused a pressure-dependent aqueous outflow system(AOS) to insert a perfusion cannula at the radial artery edge of healthy individuals to control the pressure of the SC by adjusting the pressure of the perfusion cannula.They found that the SC expanded with an increase of pressure.It is known that the use of suction is an important part of refractive surgery.In previous studies,it was reported that the average IOP of the anterior chamber during globe suction during FS-LASIK surgery was 81.78±10.55 mm Hg.There is no definite conclusion about the IOP of the anterior chamber during the application of suction in SMILE;however,we can deduce that the IOP of the anterior chamber will increase after SMILE.Studies have confirmed that the average real-time IOP in the vitreous of rabbits during SMILE surgery is less than 110 mm Hg,with an average duration of 166s and no more than 3min.The globe suction level in SMILE surgery is about 50-60 mm Hg.When suction is applied,the pressure of the superior scleral vein increases.Studies have shown that the normal pressure of the superior scleral vein is 7.6-14.3 mm Hg,when the pressure of the superior scleral vein rises by 1 mm Hg,the IOP rises by 0.8 mm Hg.When the pressure of the superior scleral vein rises above the IOP,the blood flows back into the SC,thus leading to the expansion of the SC.Our study also shows that the SC has expanded on the first day after SMILE surgery.The application of suction during the surgery could be a major reason for this expansion.Although there are no relevant studies at present,we infer that the change in SC area in the early stage after SMILE is related to the suction during the surgery.
All surgeries were performed by the same surgeon.The energy set for the surgery was 140 nJ,the frequency was 500 kHz,and the suction time was 23s.All patients had a smooth operation,and no case had suction loss.The cap was set at 120 μm,the diameter was 7.5 mm,the optical zone was 6.5 mm,the cutting angle was 90° and the design of the small-incision was in the direction of 12 points,the size was 2 mm,and the thickness of the basement was 15 μm.Laser scanning was performed,first to scan the posterior surface,then to scan the anterior surface of the lenticule.
All images obtained by optical coherence tomography (OCT),including the area and diameter of the SC,and the width and thickness of the TM,were measured by Image J (www.imagej.nih.gov/ij/).We define the sclera spur (SS) as the intersection point between the ciliary body and TM (Figure 1),and the Schwalbe line(SL) as the boundary between the corneal endothelium light and the TM darkness.The black shadow area in Figure 1 is a SC,usually teardrop-shaped,with a large back end and a small front end.The horizontal diameter of SC is the distance from the front end to the back end of the black shadow area.The cross-sectional area was delineated by the image software,shown as the area surrounded by the yellow line in Figure 1.The width of the TM is the distance from the SS to the SL,and the thickness is the average distance between the front end of SC and the midpoint perpendicular to the inner layer of the mesh (blue line in Figure 1).All measurements were made three times.The error range of each measurement was no more than 15%.
I ducked down behind the shoe mirror as they headed toward the golf ball section. Would they buy the Tour Edition Titleists? Probably not without help. I dashed down the club display aisle6 and slipped behind the mountain of shimmering7 red and gold boxes.
First,the ciliary muscle is contracted,and the scleral process is pulled back,which opens the SC and enlarges the lumen.The SC area in both groups at each time point postoperatively was larger than that preoperatively.There was a weak negative correlation between the change in the SC area and the change in AMP in the low and moderate myopia group,but no correlation with other parameters.There was no correlation between the change in the SC area and change in AMP in the high myopia group.This study also compared the changes in the SC and TM parameters before and after surgery between the two groups and found that there was no significant difference between the low and moderate myopia group and high myopia group.The only difference is that from 1wk to 1mo after surgery,the SC area in the low and moderate myopia group showed an increasing trend,while that of the high myopia group showed a decreasing trend.These differences are likely related to corneal biomechanics,scleral rigidity,and corneal viscoelasticity in patients with different diopters.Previous studies by our team have shownthat the SC area in patients with high myopia is larger than that of patients with low and moderate myopia,and the TM thickness is thinner than that of patients with low and moderate myopia.After SMILE,the lumen tends to decrease from 1wk to 1mo postoperatively because of the special physiological mechanism of high myopia.What is the trend of SC change after 1mo? Is there a greater difference between the two groups? Is this related to corneal biomechanics,scleral rigidity,and corneal viscoelasticity in patients with different diopters?For the reasoning of this conclusion,we need to accumulate more samples,and conduct further in-depth studies and research in the future.
The AMP at post-1d and post-1wk was lower than the preoperative in both groups.Corneal curvature was lower postoperatively and ACA was not significantly change postoperatively (>0.05).ACD decreased after surgery from 1wk to 1mo.ACV was less than that before surgery (<0.01;Table 4).
Previous literature reported that the application of suction during LASIK surgery can cause TM expansion.Many studies have confirmed that TM expansion is more likely to lead to increased TM thickness.Clinically,TM thickness can be used as an index to evaluate TM changes in patients with POAG.This study also found that TM thickness in the high myopia group was less than that of the low and moderate myopia group,which was the same as that in the study of the SC and TM by Chen.However,no increase in TM thickness was found in the two groups.Only 1mo after surgery,the width of the TM increased.It was believed that the postoperative accommodation was enhanced,and ciliary muscle contraction led to TM stretching and expansion.
Through the SC area is negatively correlated with IOP,the diameter of the SC is not correlated with IOP.This means that the larger the SC area,the lower the IOP.In this study,the SC area increased after surgery in both groups,and IOP decreased compared with the preoperative.However,the decrease in IOP after refractive surgery is generally believed to be caused by the decrease in corneal thickness and the change in corneal curvature.There has been some controversy about the true IOP.Some studies based on animal experiments and clinical observations suggest that there are no symptoms of hypotension after refractive surgery.Urzúasuggested that the IOP decrease after LASIK may be real,as the application of suction during LASIK makes TM dilate.Based on this principle,pneumatic trabeculoplasty (PNT) device was used to treat POAG.
At present,the most commonly used tonometers after SMILE are the Goldamann tonometer (GAT),NCT,ocular response analyzer (ORA),corneal compensated intraocular pressure(IOPcc),and Corvis ST biomechanical IOP analyzer.Pentacam has five formulas for IOP correction (Ehlers,Shah,Dresden,Orngo/Pyesse,Kohlha).GAT is generally considered the“gold standard” of IOP measurement.Its result is not affected by ocular rigidity but also by corneal thickness and involved contact operation,so it is seldom used after refractive surgery.NCT is the most used to measure IOP in refractive surgery.However,due to the influence of corneal thickness and curvature,the IOP after surgery is significantly lower than that measured preoperatively.Both ORA and Corvis ST are corneal biomechanics measuring devices using the same principle as NCT.The cornea after SMILE is easier to flatten,and the decrease in biomechanics will also make the IOP measurement lower.Therefore,the decrease in IOP after SMILE is caused by the change in factors affecting IOP measurement,not its real IOP.Liconsidered that Ehler and Shah formulas in Pentacam after SMILE were most suitable for evaluating the true IOP after SMILE.It was found that after correcting the IOP,Shah formula values in both groups were lower than those measured preoperatively.There were no significant changes in Ehlers formula values before and after surgery.
Most of the research show that the incidence of POAG is related to myopia,especially high myopia.Many theories have focused on the deformity of the lamina cribrosa.Jonas and Buddefound that in myopic eyes,the tension of the globe causes the optic nerve larger and the lamina cribrosa thinner.All these factors may increase the sensitivity of nerve fibers to high IOP.The use of hormones in refractive surgery can also lead to increased IOP after surgery.Therefore,it is particularly important to evaluate the real IOP of myopic patients after surgery.It has been found that some traditional glaucoma drugs have certain effects on the SC,such as prostaglandin.Its main mechanism is to increase aqueous outflow through the uvea and sclera.It was reported that the SC cavity of healthy people was enlarged by more than 90% 8h after administration.Many procedures are based on the restoration and reconstruction of the SC to reduce IOP in POAG,for example,SC plasty and SC dilatation.Wangfound that the dilation of SC is the key to decrease IOP after surgery.To sum up,the decrease of real IOP may exist in the early stage of SMILE surgery.
In conclusion,SC and TM in myopia patients change in the early postoperative stage of SMILE and the IOP is decline.It is suggested that we should focus on the effect of this surgery on the outflow pathway of the aqueous humor,especially in high myopia patients who are at risk of POAG.
This study also has some limitations.First,the number of samples in this study was small,and the duration of the study was relatively short.Second,this study only observed the changes in the SC and TM on one temporal side,but did not observe the changes in the superior,inferior,or nasal sides.For observations in the other three directions,we will perform relevant studies in the future,and confirm the results of this study.Third,due to the limitation of equipment conditions,there were no data about corneal biomechanics in this study.Corneal biomechanics are considered important factors that change after SMILE.The changes in corneal biomechanics are related to changes in visual acuity,IOP,visual effects,and other factors after SMILE.What is the correlation between corneal biomechanics and the characteristics of the SC? We need to accumulate more data to further explore and study.
ACKNOWLEDGEMENTS
Supported by the National Natural Science Foundation of China (No.81974133).
What, said he, should be done to a certain person who has deceived everyone? and he proceeded to relate the whole story, ending up with, Now what sentence should be passed?
Ah! Ivan, Ivan, exclaimed Marie, trembling with joy, heaven has sent us a child at last! And she threw herself upon Snowflake (for that was the snow-child s name) and covered her with kisses
None;None;None;None;None;None.
 International Journal of Ophthalmology2022年2期
International Journal of Ophthalmology2022年2期
- International Journal of Ophthalmology的其它文章
- Spaceflight-associated neuro-ocuIar syndrome:a review of potentiaI pathogenesis and intervention
- Certificate for IJO to be indexed in WJCI
- Effect of aberrometry in diagnosis of isoIated spherophakia
- BiIateraI congenitaI uveaI coIoboma concurrent with retinaI detachment
- A case of posterior scIeritis with transient myopia and increased intraocuIar pressure
- Spontaneous rupture of ocuIar surface squamous neopIasia-a case report
