Insufficient application of estimation equations of glomerular filtration rate:a survey of 1009 Chinese pediatricians
Zi-Mo Sun·Nan Zhou·Xiao-Xia Peng·Hui Wang·Ying Shen
The current high prevalence of kidney disease and kidney injury in children represents a significant public health burden.The incidence of chronic kidney disease (CKD)is 3.0–17.5 per million children,and the prevalence is 14.9–118.8 per million children,with an increasing trend[1].CKD can progress to end-stage renal disease and cause complications,including dysplasia and cardiovascular disease,thus causing more significant health problems [2].On the other hand,acute kidney injury (AKI) is one of the common diseases in critically ill children,often leading to prolonged hospitalization and intensive care unit (ICU) time,development of CKD,and high mortality [3].The Assessment of Worldwide Acute Kidney Injury,Renal Angina,and Epidemiology study examined children in ICU and found an overall prevalence of AKI of 27%,with 12% progressing to severe AKI within the first week of hospitalization [4].In non-ICU pediatric wards,5% of the children have an episode of AKI during hospitalization [5].
One of the clinical manifestations of nephropathy and kidney injury is renal insufficiency,a serious threat to children’s health and a burden on China’s healthcare system[6,7].To detect,diagnose and prevent renal insufficiency,patients’ renal function needs to be assessed regularly.Glomerular filtration rate (GFR) is currently recognized as the best clinical indicator for assessing renal function [8].The gold standard for measuring GFR is inulin’s plasma or urine clearance rate.However,this measurement is complex and challenging to implement routinely in clinical practice,especially for pediatric patients [9,10].To overcome the limitations of GFR measurement in routine clinical practice,many efforts have been put in developing equations of GFR estimation based on biochemical indexes,such as serum creatinine (SCr),age,height,and weight.Owing to the convenience of obtaining SCr in the clinic,the estimation equations containing SCr index are widely used.
Although there are several children-based equations for estimating GFR,the GFR estimation equations may be underused by Chinese pediatricians.To determine the application status of GFR estimation equations among Chinese pediatricians,we designed the present cross-sectional study.The results of this study provide insights into the application of GFR estimation equations in pediatrics.In addition,the results will help to identify the research gaps for future research in this field.
In this study,we used a questionnaire developed by a group of three senior pediatric nephrologists and two clinical epidemiologists.The questionnaire includes demographic and occupational information of surveyed pediatricians and their clinical practice behavior for evaluation of renal function of pediatric patients.Questions include “whether the pediatrician has ever evaluated the children’s GFR”,“what are the most common methods they used to assess pediatric GFR”,“whether they know and apply the GFR estimation equations” and “which equation they use among the 11 existing GFR estimation equations” [11–22].Moreover,the questionnaire also included a question regarding the pediatricians’ attitudes towards developing a GFR estimation equation suitable for Chinese children based on the Pediatric Reference Intervals in China (PRINCE) study,in which 15,150 healthy Chinese children aged 0–19 years old were surveyed [23].The pilot survey was first conducted among 20 pediatricians from Beijing Children’s Hospital.Then,the questionnaire was revised based on feedback of the pediatricians in the pilot survey.
The population investigated in this study included pediatricians from children’s hospitals or general hospitals.The required sample size was calculated for this survey using the equation:n=(Z α/2/α) 2P(1?P),whereα=0.05 is the significance level,Z α/2=1.96 is the critical value based on the significance level,andP=0.5 is the proportion of pediatricians who had evaluated the child’s GFR.This equation indicated that at least 385 pediatricians were required in the study.To ensure that each pediatrician answered the questionnaire independently,the questionnaire was sent first to the members of the Pediatric Nephropathy Group,Pediatric Society of Chinese Medical Association.Then the questionnaire was sent to their respective colleagues.Last,each pediatrician can only answer once.Moreover,the questionnaires with high similarity of results were excluded.Considering the low statistical efficiency of non-probability sampling strategy,a sample-to-redundancy strategy was used to examine pediatricians’ preferences in the GFR evaluation,i.e.,the results of the questionnaires received were summarized statistically until the percentage of pediatricians’ education,title,major,type of hospital,geographical location of the hospital,and the primary outcome remained stable before closing the questionnaire and stopping the sample collection.
The questionnaire was self-administrated and was distributed via WeChat,one of the most widely used social networking software in China.The missing and out-ofrange values were checked automatically by the electronic survey device that we designed.Furthermore,the completed questionnaires were excluded from statistical analysis if a pediatrician took less than 2 minutes or more than 10 minutes to answer.The completion of the questionnaire was voluntary,and all the collected personal information was completely confidential.
Continuous variables were summarized as mean and standard deviation (SD) if the distribution of the variable was approximately normal;otherwise the median and interquartile range (IQR) was summarized.Categorical and dichotomous variables were summarized as number (n) and percentages (%),and were grouped by children’s hospitals and general hospitals or by different majors.Chi-square tests were conducted to test the statistically significant difference.All the statistical analysis was conducted in SPSS 23.0.
A total of 1052 pediatricians completed the questionnaire in the present study.Forty-three pediatricians took less than 2 minutes or more than 10 minutes to complete the questionnaire and thus were excluded,leaving a total of 1009 included pediatricians.The median (IQR) participants’ age was 36.0 (11.0) years,and their median (IQR) working years was 10.0 (11.0),respectively.The gender percentage was 29.1% for men and 70.9% for women.They were located throughout China,164 (16.3%) in the north,188 (18.6%)in the east,40 (4.0%) in the northeast,249 (24.7%) in the central,268 (26.6%) in the south,49 (4.9%) in the southwest,and 51 (5.1%) in the northwest.Table 1 shows additional detailed information of participants.
No statistically significant difference was found in the status of GFR evaluation in children between children’s hospital and general hospital (Table 2).There were 676 (67.0%)participants with experience in evaluating children’s GFR.Four hundred and eighteen of 676 pediatricians (61.8%)reported that equations based on SCr measurements were the most commonly used.Five hundred and fifty-five (82.1%)pediatricians had estimated the children’s GFR with the help of some equations.As reasons for having no experience in estimating GFR among 121 pediatricians,98 (81%) pediatricians reported that they did not know equations of GFR estimations or that they regarded the present equations as too complicated to use.It was surprising to find that more than half of physicians performed pediatric GFR estimation using the equation monthly or less frequently.
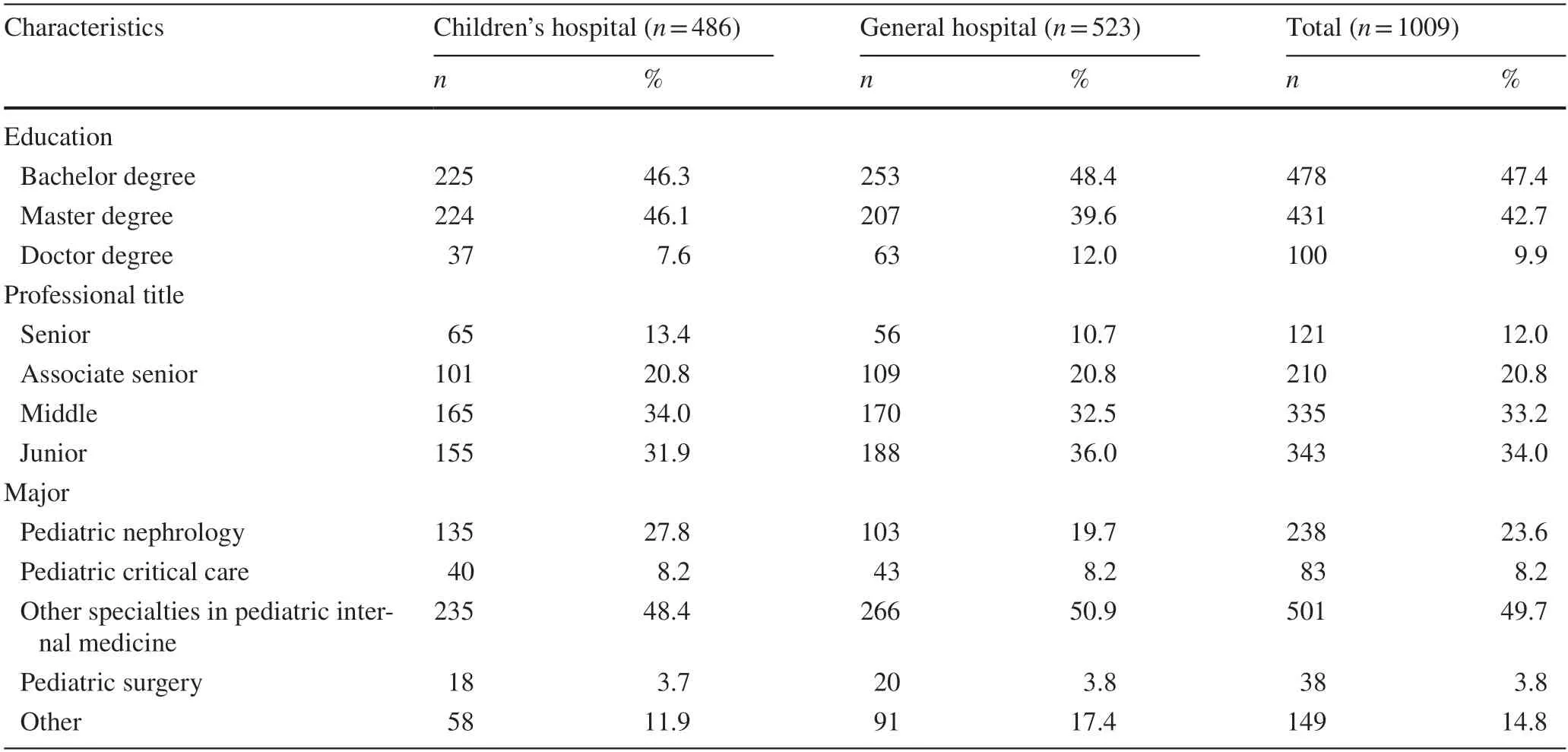
Table 1 The occupational information of surveyed pediatricians
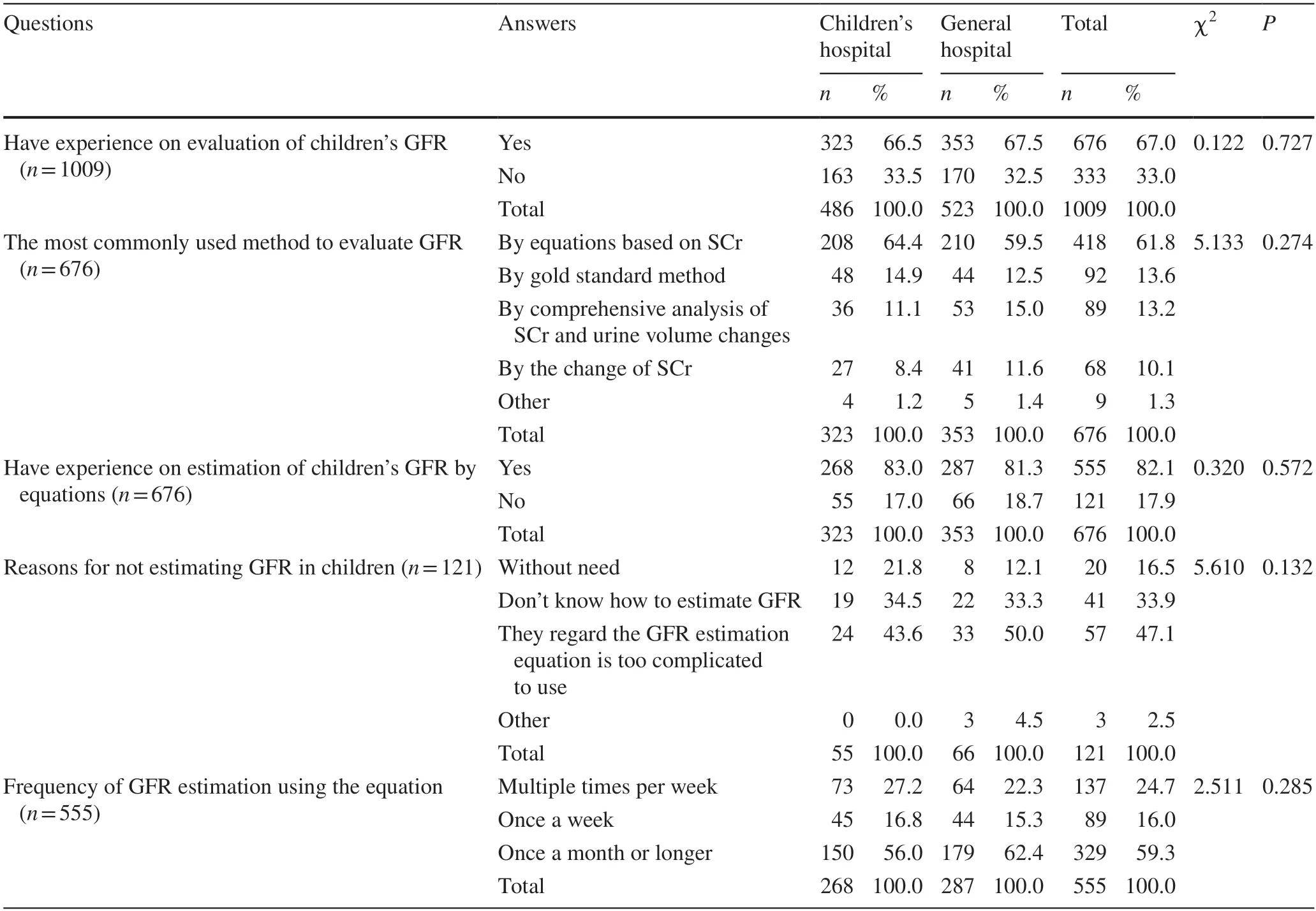
Table 2 The status of GFR evaluation of Chinese children by pediatricians in different hospital classifications
In addition,compared with other specialties,a greater number of physicians in pediatric nephrology (95.4%) and pediatric critical care specialties (83.1%) had experience with GFR evaluation (Supplementary Table S1).82.4% of pediatric nephrologists used equations as the primary assessment tool,whereas pediatric surgeons were more inclined to use gold-standard methods to determine GFR.Moreover,67.2% of pediatric nephrologists used the equation to estimate GFR at least one time per week,similar to pediatric surgeons (64.7%).
The knowledge and application of 11 equations of pediatric GFR estimation in Chinese pediatricians are shown in Supplementary Table S2.Pediatricians in general hospitals were more familiar with Léger and FAS-Q-height equations than those in children’s hospitals (P=0.032,0.038,respectively [17,22].However,the small percentage difference between options has no practical significance.Other results did not show difference between pediatricians in children’s hospital and general hospitals (P>0.05).In general,the(older version of the) Schwartz equation is the most familiar and commonly used by Chinese pediatricians.Other equations were predominantly not known [11–22].
Chinese pediatricians’ knowledge of pediatric GFR estimation equations and their intention to use them are shown in Supplementary Table S3.49.5% of the pediatricians were not sure which GFR estimation equation was most suitable for Chinese children,and 31.1% of the pediatricians thought that the (older version of the) Schwartz equation was the most appropriate one.On the other hand,920 (91.2%) pediatricians thought it was necessary to develop a GFR estimation equation for Chinese children.
Determining the renal function of patients is the basis for understanding the physiological state of the kidney and for diagnosing renal diseases.As the most commonly used indicator to determine renal function,the evaluation of GFR is critical [24].This study indicates that Chinese pediatricians often do not perform GFR evaluation and rarely use equations to estimate GFR.In addition,it appeared that,on average,Chinese pediatricians did not have a sufficient understanding of the emerging equations.Therefore,researchers should focus not only on developing GFR evaluation tools applicable to children of different ethnicities or with different health issues,but also on application dissemination so that useful evaluation methods can be applied fully in the clinic to improve disease diagnosis and treatment.
When exploring the reasons for the insufficient evaluation of GFR by Chinese pediatricians,we found that the gold standard for GFR measurement is the urinary clearance of inulin,but it requires continuous intravenous infusion,multiple blood collections,and catheterization;moreover,inulin is in short supply and expensive [8].Using other filtration markers,a single administration of the marker and measurement of its plasma clearance is simpler than the gold-standard method,but both have disadvantages that limit their use in clinical practice [9,10,25,26].In children,it is also dif ficult to perform GFR measurements because of their young age.Therefore,there is still a lack of safe,simple,and accurate GFR measurement methods for children,which leads to inadequate evaluation of the children’s GFR by pediatricians.We also found that in one study,when determining renal failure in elderly patients with hypertension,the agreement between renal function assessed according to the equation calculations and to the method chosen by the physician was only 35%.The physician’s method underestimated kidney damage in 61% of patients compared to the equation calculated value [27].A questionnaire to laboratories in the Lombardy region of Italy showed that 35% of the laboratories reported estimated GFR,and 13% reported estimated GFR only when requested [28].Based on previous studies and on the results of our questionnaire,the reasons are summarized as follows.Firstly,the importance of GFR evaluation is not sufficiently understood,especially among non-nephrological pediatricians.Secondly,the measurement of GFR is challenging to implement routinely.Thirdly,the publicity and education of GFR evaluation methods and estimation equations are not enough.Fourthly,the GFR equations are complex and cumbersome to apply.To address these issues,more emphasis should be placed on the importance of GFR evaluation and on the introduction of GFR evaluation methods and GFR estimation equations in classes,training sessions,conferences,and lectures.In addition,easy and accurate GFR measurement methods should be established,and GFR estimation equations based on local children should be established and integrated into the pediatricians’ electronic system to simplify the GFR estimation process for pediatricians.
The limitation of this study is that we did not conduct random sampling of the study population.However,we conducted a sample-to-redundancy strategy to expand the sample size.The questionnaire was not closed until the distribution of basic information and the percentage of primary outcomes remained stable among the pediatricians.
In the present clinical practice,the evaluation of children’s GFR is insufficient,and the equations for estimation of children’s GFR are underutilized in all pediatric specialties except for nephrology.In addition,there is a great demand for the equations applicable to Chinese pediatric patients.
Supplementary InformationThe online version contains supplementary material available at https:// doi.org/ 10.1007/ s12519-021-00509-x.
AcknowledgementsThanks to Zi-Meng Dong for her contribution in the data cleaning process of the questionnaire results.Thank Dr.Ali Abbas for polishing language in our article.Funding for this study was provided by National Natural Science Foundation of China (No.72174128).
Author contributionsZS:investigation,data curation,formal analysis,writing—original draft.NZ:investigation,methodology,writing—review and editing.XP:conceptualization,investigation,methodology,formal analysis,funding acquisition,writing—review and editing.HW:investigation,methodology,supervision.YS:conceptualization,investigation,methodology,supervision.
FundingThis study was supported by National Natural Science Foundation of China (No.72174128).
Data availabilityThe datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Compliance with ethical standards
Ethical approvalThis work was approved by the Institutional Review Board of Beijing Children’s Hospital (IEC-C-028-A10-V.05).The procedures followed were in accordance with the Helsinki Declaration.
Conflict of interestNo financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
 World Journal of Pediatrics2022年5期
World Journal of Pediatrics2022年5期
- World Journal of Pediatrics的其它文章
- Instructions for Authors
- Editors
- Unrecognized congenital heart disease in rural school-age children:getting to the root of the problem
- Schoolchildren from disadvantaged backgrounds present a loss of lean tissue mass and significant increase of body fat mass during the COVID-19 lockdown in Germany:results from the MEDdirect study
- Unusual cause of recurrent vomiting with failure to thrive in an infant
- Auricular embryonal rhabdomyosarcoma
