Neglected corticospinal tract injury for 10 months in a stroke patient
Neglected corticospinal tract injury for 10 months in a stroke patient
The corticospinal tract (CST) is an essential motor pathway in the human brain: particularly, it is essential for f ne hand movements (Jang, 2014). Stroke patients can show more severe weakness when a partial injury of the CST is combined with apraxia. Therefore, a thorough estimation of the CST injury degree at the beginning of stroke rehabilitation would be mandatory for a successful rehabilitation. In this study, we report on a case in whom partially injured CST had been neglected due to accompanying apraxia for 10 months.
A 71-year-old female patient was transferred for rehabilitation of hemiplegia after cranioplasty. The patient had undergone decompressive craniectomy for brain swelling due to a left middle cerebral artery (MCA) territory infarct which occurred after clipping of a ruptured left MCA bifurcation aneurysm 10 months ago at the same hospital. The patient had presented with complete paralysis (manual muscle test (Wadsworth et al., 1987): 0) of the right side (upper and lower extremities) for 10 months since the onset of cerebral infarct, although she had undergone rehabilitation at a local rehabilitation hospital for 10 months. Brain CT and brain MRI (2 days and 10 months after onset, respectively) showed a large infarct in the left MCA territory except for some portion of the left precentral gyrus (Figure 1A). The ideomotor apraxia test scores were 40 points (cut-of score < 32 points) (De Renzi et al., 1980). The patient was involved in a comprehensive rehabilitative therapy, including dopaminergic drugs for improvement of apraxia (pramipexole 1.5 mg; ropinorole 0.75 mg; amantadine 300 mg; levodopa, 750 mg) (Jang, 2013). During 3 weeks of rehabilitation treatment, the patient exhibited significant motor improvement in the right side (upper and lower extremities) to the extent that she was able to move against gravity (manual muscle test: 3). The patient provided signed, informed consent and our hospital review board approved the study protocol.
Diffusion tensor imaging (DTI) data were acquired once (10 months after onset) using a 6-channel head coil on a 1.5 T Philips Gyroscan Intera (Philips Healthcare, Best, the Netherlands) with single-shot echo-planar imaging. Seventy contiguous slices (acquisition matrix = 96 × 96, reconstructed to matrix = 192 × 192, field of view (FOV) = 240 × 240 mm2, repetition time (TR)/echo time (TE) = 10,398/72 ms, SENSE factor = 2, echo planar imaging (EPI) factor = 59, b = 1,000 s/mm2, number of excitations = 1, thickness = 2.5 mm) were acquired. Fiber assignment continuous tracking (FACT) algorithm was used for f ber tracking. The CST was reconstructed using f bers passing through two regions of interest (ROIs) on the color map. The f rst ROI and second ROI were given on the blue portion (anterior) of the upper and lower pons, respectively on the axial image of the color map (threshold fractional anisotropy = 0.15, angle = 27). The left CST was narrowed compared with the right CST; however, the integrity was preserved from the cerebral cortex to the medulla (Figure 1B).
Transcranial magnetic stimulation (TMS) was carried out using a Magstim Novametrix 200 magnetic stimulator (Novametrix Inc., Wallingford, CT, USA) at 10 months after onset. Cortical stimulation was performed (left hemisphere: a counterclockwise direction; right hemisphere: a clockwise direction). Motor-evoked potentials (MEPs) were recorded from the right thumb muscle (abductor pollicis brevis) upon stimulation of the left hemisphere with 90% of maximal output (the MEP of shortest latency; latency: 23.7 ms, amplitude: 100 μV, excitatory threshold: 70%).
In this patient, some portion of the left precentral gyrus, which is the essential origin of the CST, was preserved on 2-day brain CT and 10-month brain MRI, thus it appeared that the left CST integrity had been preserved since the left MCA infarct (Jang, 2014). In addition, MEP, which has the characteristics of the CST, was evoked at the right hand muscle on 10-month TMS (Rossini et al., 1994). Therefore, we believe that the left CST, which was partially damaged by the MCA infarction, had been in limb apraxia state for 10 months since the onset. Limb apraxia is a common disorder of skilled purposive movement; three types of limb apraxia have been reported: ideational apraxia, ideomotor apraxia, and limb-kinetic apraxia (Leiguarda and Marsden, 2000; Ochipa and Gonzalez Rothi, 2000; Hong et al., 2012; Jang, 2013). Limb-kinetic apraxia is attributable to injury of the premotor cortex with preservation of CST integrity (Leiguarda and Marsden, 2000; Ochipa and Gonzalez Rothi, 2000; Hong et al., 2012; Jang, 2013). Precise diagnosis of limb-kinetic apraxia is dif cult because it is made by clinical observation of movements without use of specif c evaluation tools (Hong et al., 2012; Jang, 2013). In this patient, brain MRI f ndings involving the fronto-parietal cortex suggested the possibility of limb-kinetic apraxia and ideomotor apraxia; however, because the patient showed an intact ideational plan for motor performance in the ideomotor apraxia test, we think that the motor improvement for 3 weeks since 10 months after onset was mainly attributed to the resolution of limb-kinetic apraxia (De Renzi et al., 1980). Our results suggest the importance of thorough evaluation of the damage degree of the tracts at the beginning of stroke rehabilitation. However, limitation of using DTI in this study should be taken into account. Fiber tracking is an analyzer dependent method. In addition, DTI might underestimate the neural f bers due to the f ber-crossing ef ect (Lee et al., 2005; Yamada et al., 2009).
This work was supported by the DGIST R&D Program of the Ministry of Science, ICT and Future Planning (15-BD-0401). SHJ designed this study, collected and analyzed data, and revised the paper. CHC participated in study design and data collection. WHJ participated in data collection and analysis and wrote the paper. All authors approved the f nal version of this paper.
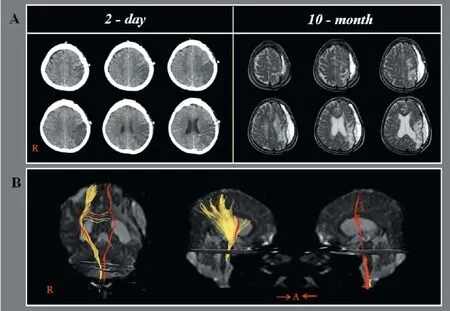
Figure 1 CT, T2-weighted MRI and dif usion tensor tractography (DTT) images in a stroke patient.
Sung Ho Jang, Chul Hoon Chang, Woo Hyuk Jang*
Department of Physical Medicine and Rehabilitation, College of Medicine, Yeungnam University, Daemyungdong, Namku, Daegu, Republic of Korea (Jang SH, Jang WH)
Department of Neurosurgery, College of Medicine, Yeungnam University, Daemyungdong, Namku, Daegu, Republic of Korea (Chang CH)
*Correspondence to: Woo Hyuk Jang, M.S., wlqtksek@hanmail.net.
Accepted: 2015-09-28
orcid: 0000-0002-7012-4565 (Woo Hyuk Jang)
De Renzi E, Motti F, Nichelli P (1980) Imitating gestures. A quantitative approach to ideomotor apraxia. Arch Neurol 37:6-10.
Hong JH, Lee J, Cho YW, Byun WM, Cho HK, Son SM, Jang SH (2012) Limb apraxia in a patient with cerebral infarct: dif usion tensor tractography study. NeuroRehabilitation 30:255-259.
Jang SH (2013) Motor recovery by improvement of limb-kinetic apraxia in a chronic stroke patient. NeuroRehabilitation 33:195-200.
Jang SH (2014) The corticospinal tract from the viewpoint of brain rehabilitation. J Rehabil Med 46:193-199.
Lee SK, Kim DI, Kim J, Kim DJ, Kim HD, Kim DS, Mori S (2005) Diffusion-tensor MR imaging and f ber tractography: a new method of describing aberrant f ber connections in developmental CNS anomalies. Radiographics 25:53-65.
Leiguarda RC, Marsden CD (2000) Limb apraxias: higher-order disorders of sensorimotor integration. Brain 123:860-879.
Ochipa C, Gonzalez Rothi LJ (2000) Limb apraxia. Semin Neurol 20:471-478.
Rossini PM, Barker AT, Berardelli A, Caramia MD, Caruso G, Cracco RQ, Dimitrijevic MR, Hallett M, Katayama Y, Lucking CH, et al. (1994) Non-invasive electrical and magnetic stimulation of the brain, spinal cord and roots: basic principles and procedures for routine clinical application. Report of an IFCN committee. Electroencephalogr Clin Neurophysiol 91:79-92.
Wadsworth CT, Krishnan R, Sear M, Harrold J, Nielsen DH (1987) Intrarater reliability of manual muscle testing and hand-held dynametric muscle testing. Phys Ther 67:1342-1347.
Yamada K, Sakai K, Akazawa K, Yuen S, Nishimura T (2009) MR tractography: a review of its clinical applications. Magn Reson Med Sci 8:165-174.
10.4103/1673-5374.172327 http://www.nrronline.org/
Jang SH, Chang CH, Jang WH (2015) Neglected corticospinal tract injury for 10 months in a stroke patient. Neural Regen Res 10(12):2060-2061.
 中國(guó)神經(jīng)再生研究(英文版)2015年12期
中國(guó)神經(jīng)再生研究(英文版)2015年12期
- 中國(guó)神經(jīng)再生研究(英文版)的其它文章
- Neuroplasticity in post-stroke gait recovery and noninvasive brain stimulation
- Structural and functional connectivity in traumatic brain injury
- Polyurethane/poly(vinyl alcohol) hydrogel coating improves the cytocompatibility of neural electrodes
- Transplantation of human telomerase reverse transcriptase gene-transfected Schwann cells for repairing spinal cord injury
- Electroacupuncture promotes the recovery of motor neuron function in the anterior horn of the injured spinal cord
- A novel method for evaluating brain function and microstructural changes in Parkinson’s disease
