The role of percutaneous hepatic perfusion (PHP) in the treatment of cholangiocarcinoma
Cornelia L.A.Dewald, Arndt Vogel, Frank K.Wacker
1Department of Diagnostic and Interventional Radiology, Hannover Medical School, Hannover 30625, Germany.
2Department of Gastroenterology, Hepatology and Endocrinology, Hannover Medical School, Hannover 30625, Germany.
3Division of Gastroenterology and Hepatology, Toronto General Hospital, Toronto, ON M5G 2C4, Canada.
Abstract This review article evaluates the current literature on the role of percutaneous hepatic perfusion (PHP) as a treatment option in cholangiocarcinoma (CCA).CCA is a rare cancer that is mostly diagnosed at a late stage.Patients with advanced, unresectable disease have limited treatment options.PHP is a locoregional therapy that delivers high doses of chemotherapy directly to the liver while minimizing systemic exposure and toxicity.This review allocates PHP in the therapeutic spectrum of CCA and summarizes the available literature with a focus on the clinical efficacy and safety profile.Results from studies evaluating the efficacy and safety of PHP are promising,with several observational studies demonstrating improvements in progression-free survival and overall survival rates.However, PHP is not without side effects; the most commonly reported adverse events include transient hematotoxicity and hepatotoxicity.PHP has the potential to be a valuable treatment option for patients with unresectable CCA.Nonetheless, further trials are needed to optimize patient selection, treatment regimens, and long-term outcomes.
Keywords: Cholangiocarcinoma, intraarterial therapies, percutaneous hepatic perfusion, locoregional therapy
INTRODUCTION
Cholangiocarcinoma (CCA) is a rare form of cancer that affects the biliary tract.It is the second most common primary liver malignancy and can be classified as intrahepatic (iCCA) or extrahepatic (eCCA)tumors, which are further divided into distal and perihilar carcinomas (also known as Klatskin carcinomas)[1].This distinction is relevant due to differences in, e.g., different risk factors, clinical characteristics, and varying therapeutic approaches.For instance, while primary sclerosing cholangitis represents a significant risk factor for both iCCA and eCCA, the presence of liver cirrhosis significantly increases the risk of developing iCCA[2].Pre-existing comorbidities (such as cirrhosis) undoubtedly exert a significant influence on the prognosis, which is generally poor in CCA, with five-year survival rates of less than 5% in unresectable disease and 33% in resectable disease[3-6].
Accurately distinguishing iCCA can pose a challenge.On contrast-enhanced dynamic cross-sectional imaging, up to 81% of iCCA cases exhibit a pattern of contrast enhancement that progresses from the arterial to the venous phase, particularly prominent in the late phase.In contrast, hepatocellular carcinoma(HCC) is characterized by arterial hypervascularization during the arterial phase and washout in the venous phase or late phase.However, some small iCCA may also show arterial hypervascularization and may thereby mimic HCC[4].
Surgery is the preferred treatment for localized disease, but most patients present with advanced,unresectable tumors at first diagnosis.In these patients, the primary first-line chemotherapy is the combination of gemcitabine and cisplatin, which is based on the phase III ABC-02 trial[7].More recently, the phase II GAP trial explored the inclusion of nab-paclitaxel alongside gemcitabine and cisplatin for first-line therapy.Promising initial results have prompted anticipation for the phase III trial results[8].In terms of second-line systemic therapy, the phase III ABC-06 trial has established the standard of care with FOLFOX[9].There have also been recent developments in various targeted and immunomodulating therapies.An example is the anti-PD1 monoclonal antibody Pembrolizumab for the treatment of solid tumors with high microsatellite instability (MSI-H)[10].
Alarmingly, according to a recent systematic review[11], the evidence for therapeutic decisions for patients with advanced CCA stems from only a few randomized control trials with a low degree of robustness.As the incidence of CCA continues to rise, there is a growing need for effective therapies.
In liver-dominant disease, locoregional therapies (LRT) are an integral part of the treatment portfolio for local tumor control and overall survival (OS) improvement[12].LRT address tumor growth and its local complications, mainly tumor-related liver failure, which is a prevalent death cause in patients with iCCA.Studies using LRT alone and in combination with systemic chemotherapy resulted in a survival benefit,especially in patients who could be down-staged to (R0-) resection[2].In a recent systematic review and pooled analysis, radioembolization (TARE), transarterial chemoembolization (TACE), and hepatic arterial infusion (HAI) demonstrated a pooled mean weighted OS of 15.7 months, with a longer OS of 25.2 months for patients treated with concomitant systemic first-line chemotherapy[13].
However, since most of the literature on LRT for iCCA is based on single-center retrospective trials, the data are diverse and lack sufficient quality to formulate robust recommendations.Hence, Edelineet al.conclude that their analysis is limited by the large heterogeneity of the study results.There is a recognized gap in prospective evidence, particularly from randomized controlled trials (RCTs), regarding the use of LRT in patients with iCCA.They also confirm that future research seems justified by the encouraging results presented in their systematic review[13].Moreover, it appears essential to conduct RCTs that compare the various LRT not only in iCCA but also in CCA liver metastases.These trials can provide valuable insights into identifying the patients who derive the greatest benefit from specific treatments or treatment combinations.
Percutaneous hepatic perfusion (PHP) is a relatively new locoregional procedure that delivers high doses of chemotherapy directly to the liver while minimizing systemic exposure and toxicity.This review article will evaluate the role of PHP in the treatment of iCCA and eCCA metastases and discuss the available data regarding its efficacy and safety.
LOCAL AND LOCOREGIONAL THERAPIES
Local and locoregional treatment options include percutaneous ablation procedures and intraarterial approaches such as conventional or drug-eluting bead chemoembolization (cTACE and debTACE), TARE,and regional high-dose local chemotherapies such as HAI and PHP.
Percutaneous tumor ablationtechniques involve the use of various methods such as radiofrequency (RFA)or microwaves (MWA), laser or cryotherapy, the injection of chemicals like ethanol, or irreversible electroporation[10].These focal treatment methods are typically reserved for patients with a limited number of small tumors in patients not eligible for surgery or for small recurrent tumors after surgical resection.
TAREinvolves the supraselective injection of radioactive microspheres into the hepatic artery to deliver a high dose of radiation to liver tumor cells while minimizing damage to healthy tissue[14,15].Trials have documented median survival times spanning from 9 to 22 months[14].
TACEis another treatment option that can deliver chemotherapy directly to the diseased tissue while minimizing damage to the healthy liver tissue.Studies have shown that TACE in CCA can achieve a median OS of 12-17 months when used alone.An additional survival benefit of 2-12 months was reported in combination with systemic therapy[2].
HAIis a treatment that delivers chemotherapy directly to liver tumors through the hepatic artery using a surgically implanted pump[14].
PHPis a locoregional high-dose chemotherapy perfusion of the liver through a transfemoral approach.This therapy is taking advantage of the dual blood supply of the liver.While healthy/cirrhotic liver cells are supplied by both the hepatic artery and portal vein, liver tumors are perfused almost exclusively by the hepatic arteries.Thus, during PHP, the tumors are saturated with chemotherapy, whereas only a small fraction of the remaining liver parenchyma is affected, and the viability of the unaffected tissue is preserved.By temporarily isolating the liver from the systemic circulation and using an extracorporeal chemofiltration system (Delcath Systems Inc., New York, USA), systemic toxicity is effectively mitigated.In contrast to surgical hepatic perfusion, which requires extensive mobilization of the liver via a laparotomy and isolation of the inferior vena cava as well as dissection of the porta hepatis structures[16], the minimally invasive approach PHP is easily repeatable, thus offering a palliative life extension as part of an individual therapy plan.
After the introduction of the commercial filter system by Delcath Systems Inc.(New York, USA), a secondgeneration filter system with enhanced melphalan extraction rates has been accessible since 2012.Numerous single- and multicenter studies ranging from phase I to phase III have been conducted to assess the effectiveness of PHP in various tumor entities[17-19].While there is substantial and reliable data on PHP in metastatic uveal melanoma[17,20-24], investigations into the efficacy of PHP in other solid tumors, such as CCA, remain limited.Moreover, existing studies suffer from heterogeneity in patient characteristics and reporting methods.A randomized controlled phase III study is currently underway to evaluate the effectiveness, safety, and pharmacokinetic aspects of PHP after systemic therapy with cisplatin/gemcitabine compared to systemic therapy with cisplatin/gemcitabine alone.This study involves 40 PHP centers, and the results are pending (NCT03086993).
Mechanism of action
All PHP procedures are conducted in the interventional radiology suite, with the patient under general anesthesia[20-29].Two percutaneous venous access sheaths and one arterial access sheath are inserted using ultrasound guidance by the interventional radiologist.An 18 F sheath is placed in the right common femoral vein and a 10 F sheath is inserted in the right internal jugular vein (IJ).A 5 F sheath placed in the left common femoral artery is later used to advance a catheter into the superior mesenteric and the hepatic artery.DSA of the celiac trunk and indirect portograms of the superior mesenteric axis are acquired to confirm the anatomy usually known from visceral MR- or CT-angiography, and to rule out any arterial anatomic variants that would require certain catheter positions or small atypical branches originating from the hepatic arteries (e.g., left gastric), which may require coil embolization to prevent unintended chemotherapy delivery to other visceral organs.Once successful access is achieved, systemic anticoagulation using unfractionated heparin is initiated, aiming for an activated clotting time (ACT) greater than 500 sec.Anticoagulation is monitored by repeated ACT measurements throughout the procedure, and repeated doses of heparin are given, if necessary.
Subsequently, a 16 F double balloon hepatic isolation and aspiration catheter (DelcathSysytems, Inc., New York, NY) is advanced via the femoral 18 F venous sheath and positioned in the hepatic segment of the inferior vena cava (IVC).The cranial balloon of the double-balloon catheter is inflated within the right atrium and gradually retrieved until it establishes a secure seal at the junction of the IVC and the right atrium.Due to the funnel-shaped anatomy of the cavoatrial junction, the balloon takes on the shape of a cork.Subsequently, the caudal balloon is inflated and positioned below the hepatic veins and cranial to the renal veins.Side holes in the catheter between the cranial and caudal balloon allow for venous outflow of the hepatic venous blood and the isolated hepatic IVC segment to be shunted extracorporeally.In order to confirm the isolation of the hepatic segment and to exclude leakages alongside the double-balloon catheter,a digital subtraction venogram is performed by injection of contrast media through a dedicated side port of the double-balloon catheter under transient respiratory arrest.A perfusion bypass machine is employed to establish an extracorporeal veno-veno bypass.During this process, the venous hepatic blood is aspirated into a melphalan-specific filtration system, where it undergoes filtration (with filtration rates of approx.86%[25]).Then, the cleansed blood is fed back into the large circulation via the IJ venous return catheter.This completes the veno-veno bypass circuit, as illustrated in Figure 1.Prior to chemotherapy infusion into the proper hepatic artery, an angiogram is performed to confirm the catheter position and to test the flow in the hepatic artery.In case of flow-restricting vasospasm, vasodilative drugs are applied intra-arterially.Then,high doses of melphalan are delivered directly to the liver.Intra-arterial perfusion is performed for approx.30 min (wash-in phase): 500 cc of melphalan solution is infused in portions of 100 cc at a rate of 0.4 mL/s.In between the sets, a repeat angiogram is performed and vasodilative drugs can be injected if necessary.An additional 30-min period on the extracorporeal veno-veno bypass allows for the elimination of any residual drug within the liver, marking the washout phase.
Throughout the procedure, hemodynamic pressure drops are common and can be attributed to the decreased preload upon isolation of the hepatic IVC and the interposition of the filtration system.Due to the predictable decrease in arterial blood pressure, routined anesthesiologists tend to aim for systolic blood pressures above 150 mmHg prior to starting the extracorporeal circulation[28].For hemodynamic management, patients receive fluid support and vasopressor agents at the discretion of the attending anesthesiologist.
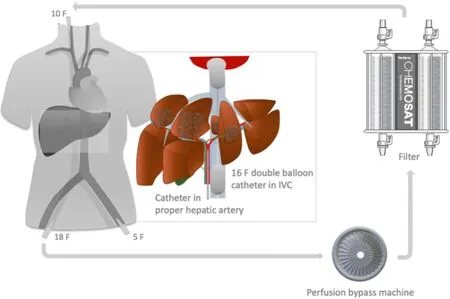
Figure 1.Overview of the PHP setup.Introducer sheaths are inserted in the left common femoral artery (5 French) and the right common femoral vein (18 French).As shown on the magnified image of the liver, a catheter is placed in the proper hepatic artery to infuse melphalan to the diseased liver parenchyma (for better visualization, catheter is not shown in a selective position).A doubleballoon catheter is inserted in the inferior vena cava (IVC).To isolate the retrohepatic segment of the IVC, the cephalic balloon is inflated at the cavoatrial junction, and the caudal balloon is inflated below the confluence of the liver veins.The catheter in between the balloons is equipped with multiple fenestrations.Using the suction forces of a bypass machine, the melphalan-enriched venous blood from the liver is pumped into an extracorporeal filtration system, which separates the melphalan from the blood before passing on the melphalan-cleansed blood to a 10 F introducer sheath placed in the right internal jugular vein for systemic return.
Melphalan, a non-cell-cycle-specific alkylating agent, is suitable for PHP treatment due to its high first-pass metabolism and rapid hepatic clearance rate[29].Although not commonly utilized in CCA[30,31], it is selected for these specific properties.The total dosage administered is max.3 mg per kilogram of the patient’s ideal body weight, ensuring appropriate adjustments for individual variations.One may wonder about the effectiveness of PHP and where it derives its efficacy from.PHP enables a significant increase in the dosage of melphalan delivered directly to the liver tumor while minimizing systemic exposure through extracorporeal filtration.Therefore, the cytotoxic alkylating impact of PHP is most probably due to the high concentration of chemotherapy reaching the tumor[1].Melphalan is the sole agent authorized for use with the extracorporeal filtration system.Its widespread availability and cost-effectiveness make it a feasible option for medical institutions[10].
Following the completion of the washout phase, patients are moved to intensive care unit, where they spend the first 12-24 h at the discretion of the interventional radiologist and the oncologist.Once their coagulation status allows it, the sheaths are removed.This step ensures the safe withdrawal of the sheaths while maintaining appropriate hemostasis and minimizing the risk of complications.The arterial puncture site is usually sealed with a closure device.
In our center, we have conducted a total of 233 PHP procedures for a variety of liver tumors, but mainly in uveal melanoma and CCA.During one PHP, we had to terminate the procedure due to clotting issues in a patient with hemophilia.This patient was rescheduled after hemostaseological consultation 2 weeks later.In another patient, the procedure had to be prematurely halted (prior to melphalan administration) after the patient developed atrial fibrillation following the insertion of a central venous line.This patient was rescheduled after cardiology consultation 4 weeks later.Furthermore, another patient could not be anticoagulated due to arterial malpuncture, so the PHP was postponed.In other high-volume centers,isolated cases of discontinuation of the procedure were reported, e.g., due to clotting within the filtration system or balloon incompatibilities[32].Nevertheless, these instances remain infrequent, affirming the overall high technical feasibility of the procedure.
Clinical efficacy
In a retrospective analysis conducted by Schoenfeldet al., 14 CCA patients (iCCA or eCCA metastases)treated with PHP were reported, with an overall response rate (ORR) of 31%, enclosing one case of complete remission and one patient with the longest OS of 3.7 years after initiation of PHP treatment[20].In an update of the cohort, comprising 17 patients with iCCA or eCCA metastases treated with 42 PHP, the OS was 27.6 months from first diagnosis and 9.9 months from first PHP.The progression-free survival (PFS)was 4 months, the ORR was 25%, and the disease control rate (DCR) was 75%[1].In another small retrospective study, 3 patients with CCA treated with 5 PHP were included and achieved a PFS of 8.3 months[33].Other studies included small numbers of patients with CCA receiving PHP but did not evaluate them separately.In 2019, Marquardtet al.reported the only multi-institutional study so far.The evaluation included 26 PHP treatments administered to 15 patients with iCCA, revealing an ORR of 20% and local disease control in 53% of patients.The median OS was reported as 26.9 months from the initial diagnosis and 7.6 months from the first PHP treatment, while the median PFS was 4.1 months.Notably, individuals with liver-only disease exhibited a significantly longer median OS compared to those with locoregional lymph node metastases (12.9 monthsvs.4.8 months, respectively)[34].
Safety and toxicity
Regarding safety, no clinically relevant adverse events during the PHP procedure are reported.However,postinterventional hematological toxicity including thrombocytopenia and anemia, requiring transfusions in the postprocedural period and transient liver enzyme elevations, were fairly common.Serious adverse events included puncture site complications, pneumonia, acute renal failure, and one case of a minor stroke[1,20,26,33,34].Furthermore, Marquardtet al.report on one patient with a tumor load > 40% of the liver that developed multi-organ failure after PHP[34].It is important to note that, according to a retrospective matched cohort study, PHP can safely be used in patients with prior hemihepatectomy[26]with dosage dependent on body weight.
CASE EXAMPLE
To demonstrate the treatment success of PHP as a treatment option even after surgical resection, we highlight a case of a female patient diagnosed with intrahepatic CCA at the age of 35.The primary tumor was treated surgically and adjuvant chemotherapy with gemcitabine and cisplatin was initiated.However,after a short time, the tumor relapsed.As part of an individual treatment plan, over the course of the next three years, the patient received a total of eight PHP treatments, leading to disease stabilization of the treated lesions.Nevertheless, new lesions, which had not been addressed with PHP, kept developing but were eligible for locoregional therapies such as MWA and radiosurgery.This combination and sequence of various treatments resulted in an overall survival of 46 months since diagnosis.Figure 2 depicts the chronological sequence of the treatments in detail.Figure 3 provides the exemplary course of the follow-up imaging controls over 1 year.Figure 4 provides angiographic images of the first PHP performed on the patient.
PROSPECTS FOR PHP
As research and technology progress, the outlook for PHP in liver disease treatment appears promising.However, its place in standard medical practice will rely on continuous scientific exploration and clinical validation.Various research groups, including our own, have initiated studies to delve into the periinterventional safety of PHP[25,28,35].A more comprehensive grasp of the anesthesiological challenges associated with PHP and peri-procedural coagulation management will be benefical for the patients.
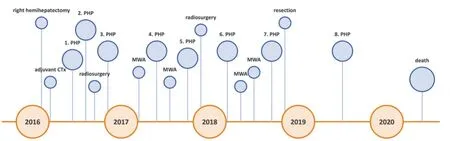
Figure 2.Chronological overview of the individual treatment plan of a 35-year-old patient with intrahepatic cholangiocarcinoma.CTx:chemotherapy; MWA: microwave ablation; PHP: percutaneous hepatic perfusion.
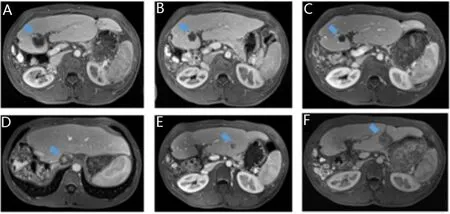
Figure 3.Consecutive MR images (T1 sequence post contrast) of a patient with intrahepatic cholangiocarcinoma, which was initially treated with right hemihepatectomy and adjuvant chemotherapy.(A) Shortly after the right hemihepatectomy the tumor relapses in segment 4b; After the first PHP treatment (B), the tumor has decreased in size and vitality; (C) following the second PHP, the treated lesion has further decreased in size, but a new metastasis, which had not been evident at time of the PHP, has developed in segment 1(D); The lesion in segment 1 is treated with radiosurgical photon therapy.The third PHP is performed and provides disease stabilization of the tumor; A new lesion in segment 3 (E) is successfully addressed with microwave ablation (F).
Ongoing and upcoming clinical trials are persistently assessing the safety and efficacy of PHP in diverse clinical contexts.Exploring combination therapies with, e.g., immunotherapy, targeted treatments, or radiation, is vital, as these combined approaches may open new avenues for improved outcomes.
In essence, robust data, ideally from randomized controlled studies, would be invaluable in comprehending PHP's effectiveness and its enduring impact.Depending on the outcomes of these studies, indications for PHP may expand and be tailored to meet the needs of individual patients.Furthermore, if PHP proves to be both effective and safe in clinical trials, it could garner regulatory approvals for broader clinical use and insurance coverage, making PHP more accessible to patients.
CONCLUSION
Although the use of PHP for treating unresectable cholangiocarcinoma is still under evaluation, findings suggest that it is a promising treatment option for patients with advanced disease.PHP has several potential advantages over other locoregional treatment options, including its ability to deliver high doses of chemotherapy directly to the liver while minimizing the toxicity on the rest of the body.However, further research is needed to fully evaluate the efficacy and safety of PHP in the treatment of cholangiocarcinoma,to assess the potential of PHP in combination with other therapies, and to identify which patients are most likely to benefit from this treatment modality.
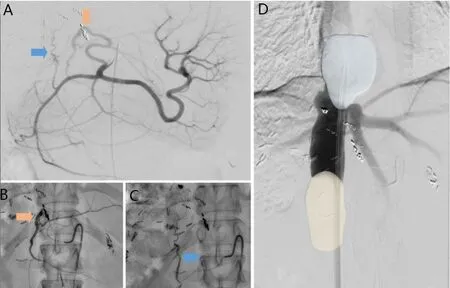
Figure 4.Angiographic images of the first percutaneous hepatic perfusion (PHP) performed in the patient.Please note, that after right hemihepatectomy, the anatomy of the upper abdomen has shifted due to the compensatory growths of the remaining liver tissue.After ultrasound-guided puncture of the left common femoral artery and insertion of a 5F sheath, a 4F diagnostic catheter is placed in the celiac trunk.(A)digital subtraction angiography (DSA) of the celiac trunk is performed.The left hepatic artery originates from the left gastric artery (orange arrow).The blue arrow marks an additional branch supplying the liver, which comes from the gastroduodenal artery; Both branches are selected as therapy positions and are successively probed using a microcatheter: (B) microcatheter-based probing of the left hepatic artery; (C) microcatheter-based probing of the additional branch coming from the gastroduodenal artery.Before administering the chemotherapy, the right common femoral vein is punctured using ultrasound-guidance.After insertion of a 18F sheath, a double balloon catheter in placed in the inferior vena cava (IVC); (D) the cranial balloon (blue) is inflated above the confluens of the liver veins and the caudal balloon (yellow) in inflated caudal the confluens.Using a dedicated side port of the double balloon catheter, a DSA of the IVC and liver veins is performed to rule out leakages alongside the balloons.Afterwards, subsequent chemotherapy infusion via the first and then second therapy position is performed.(Neither the extracorporeal circuit nor the venous return sheath placed in the internal jugular vein are depicted in this Figure.Please refer to the schematic overview in Figure 1.)
DECLARATIONS
Authors' contributions
Conceptualization: Dewald CLA, Vogel A, Wacker FK
Investigation: Dewald CLA, Wacker FK
Resources and supervision: Wacker FK
Writing-original draft preparation, methodology, and visualization: Dewald CLA
Writing-review and editing: Vogel A, Wacker FK
Reading and agreed to the published version of the manuscript: Dewald CLA, Vogel A, Wacker FK
Availability of data and materials
Not applicable.
Financial support and sponsorship
This study was supported by PRACTIS-Clinician Scientist Program, funded by the German Research Foundation (DFG, ME 3696/3-1).
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Copyright
? The Author(s) 2024.
- Hepatoma Research的其它文章
- Introduction of Chinese expert consensus on neoadjuvant therapy for primary liver cancer (2023 edition)
- Introduction to 2023 Chinese expert consensus on the whole-course management of hepatocellular carcinoma
- Reflections and perspectives on adjuvant treatment in the setting of resected hepatocellular carcinoma
- Dysmetabolic comorbidities and non-alcoholic fatty liver disease: a stairway to metabolic dysfunctionassociated steatotic liver disease
- Progression of liver disease and associated risk of hepatocellular carcinoma
- Role of temporary portosystemic surgical shunt during liver resection to prevent a post-resection small for size-like syndrome

