Role of temporary portosystemic surgical shunt during liver resection to prevent a post-resection small for size-like syndrome
Jacopo Lanari, Marina Polacco, Umberto Cillo
Department of Surgical, Oncological and Gastroenterological Sciences, General Surgery 2 Hepato-Pancreato-Biliary Surgery and Liver Transplantation Unit, Padua University Hospital, Padua 35128, Italy.
Abstract Liver resection stands as the gold-standard therapeutic approach for selected cases of hepatocellular carcinoma(HCC).The extent of resectable parenchyma hinges upon the underlying liver function and its regenerative potential.Consequently, cirrhosis may impede access to potentially curative interventions for HCC arising within this context.Cirrhotic patients undergoing liver resection face heightened susceptibility to post-hepatectomy liver failure (PHLF).The clinical profile of PHLF bears a resemblance to a well-documented syndrome within the liver transplant (LT) domain: Small-for-size syndrome (SFSS), a form of graft failure observed in the postoperative phase following LT with undersized or partial organs.Management of SFSS targets mitigating the overflow syndrome, achievable through diverse portal diversion techniques.Portal vein flow diversion encompasses procedures redirecting a variable proportion of portal vein flow towards systemic circulation.Consequently,derivative procedures aim to directly alleviate portal hypertension.Side-to-side portocaval shunts emerge as the most straightforward and efficacious means of decompressing the portal system.Furthermore, they afford flow calibration to diminish the incidence and severity of steal syndrome and hepatic encephalopathy, without compromising efficacy or hepatic function.Translating insights gleaned from LT complexities involving SFSS to liver resection, strategies involving portal flow diversion warrant consideration in efforts to forestall PHLF.This approach aims to extend the frontiers of liver surgery, broadening access to hepatectomy with curative intent, either as a standalone intervention or as part of a comprehensive treatment regimen where LT serves as a secondary option.
Keywords: Portosystemic shunts, liver resection, cirrhosis, post-hepatectomy liver failure, small-for-size
INTRODUCTION
Liver resection stands as the benchmark treatment for carefully chosen cases of hepatocellular carcinoma(HCC), contingent upon the disease stage and liver function[1,2].Surgeons prioritize considerations of tumor burden and the quality of liver tissue when strategizing hepatectomy.The volume of resectable parenchyma depends on underlying liver function and its regenerative capacity; hence, cirrhosis can limit access to potentially curative treatments of HCC arising in this context.Cirrhotic individuals undergoing liver resection face heightened susceptibility to post-hepatectomy liver failure (PHLF), wherein the future liver remnant (FLR) fails to meet the patient's metabolic demands.PHLF manifests through progressive organ dysfunction, accentuated by metabolite accumulation (bilirubin, ammonia,etc.) and complications such as ascites, hemorrhage attributable to diminished coagulation factor synthesis, septic infections, and renal impairment.The rapid progression from liver failure to multi-organ failure underscores the urgency in managing this condition to avert patient mortality[3].
Pathophysiology of post-hepatectomy liver failure
Cumulating evidence supports the hypothesis that the functional failure of the remnant liver after hepatectomy may be caused by alterations in the hepatic microvascular bed[4-8].A critical factor in this process is the wedge pressure at the sinusoidal level.In cirrhotic livers, the control mechanisms of sinusoidal flow are compromised.Relative portal hyperperfusion, characteristic of cirrhosis and exacerbated by reduced vascular bed post-hepatectomy, leads to microcirculatory trauma and subsequent inhibition of organ functions.Experimental studies indicate that while some degree of portal hyperperfusion stimulates hepatic regeneration, excessive increases may cause hepatocellular damage[9,10].
Intrahepatic flow and its composition, particularly the proportion of venous and arterial blood, are vital for organ homeostasis[11-14].The Hepatic Arterial Buffer Response (HABR) plays a key role in maintaining hepatic blood flow stability.The physiological basis of HABR involves adenosine clearance, a potent vasodilator, predominantly for the hepatic artery[15].Decreased portal flow increases intrahepatic adenosine concentration, stimulating hepatic arterial flow to maintain overall organ blood flow[12].
Conversely, increased portal flow post-hepatectomy reduces arterial supply[16], potentially impacting bile duct perfusion.Research using techniques like portal vein ligation in animal models reveals that substantial portal stenosis triggers HABR[11].
The increase in portal flow resulting from parenchyma removal causes an important decrease in the arterial supply to the organ; the consequences of this alteration lead to relative ischemia of the biliary tree and a decrease in the regenerative capacity of the liver.Microscopic changes include endothelial and sinusoidal alterations, hepatocyte degeneration, mitochondrial swelling, thrombotic events in small portal branches,occasional recanalization, regenerative hyperplasia, and biliary stenosis in later stages[11,17,18].
Limits of current strategies to increase FLR in cirrhotic patients
Understanding the significance of a small future liver remnant (FRL) and its impact on the feasibility of curative liver tumor resection has been pivotal.Strategies to increase so-calledfunctional resectabilityhave been investigated over the last 15 years[19].Portal vein embolization (PVE) or ligation (PVL) stands out as a significant advancement, enabling preoperative modulation of liver volume.The evolution of this concept has led to two-stage hepatectomy (TSH) and, more recently, associated liver partition and portal vein ligation for staged hepatectomy (ALPPS).These techniques have facilitated extensive hepatectomy, even for multiple or large HCCs, by augmenting the FLR[20,21].However, the efficacy of liver volume modulation varies across different liver malignancies and is contingent upon liver parenchyma quality.TSH is hampered by an incompletion rate of over 30%, attributed to ineffective liver hypertrophy and potential tumor growth stimulation[22,23].ALPPS initially promised nearly 100% resection rates for otherwise functionally irresectable tumors[24,25], but enthusiasm waned due to high morbidity and mortality rates,particularly in HCC patients[26,27].The exact underlying causes remain elusive; however, the prolonged manipulation and permanence of the tumor for several days after the first-stage operation, coupled with a surge in cytokines and growth factors postoperatively, have been implicated in inter-stage tumor progression[26,28].Moreover, FLR hypertrophy in fibrotic/cirrhotic livers appears suboptimal compared to noncirrhotic counterparts[29].This concept is also reinforced by the evidence that the outcomes improved from the early phase, in which ALPSS was carried out in HCC patients regardless of the degree of underlying cirrhosis or concomitant portal hypertension[30], compared to the current era, when more stringent criteria are applied[31,32].Consequently, advanced cirrhosis and portal hypertension emerge as limiting factors for liver volume modulation techniques.
Similarities between post-hepatectomy liver failure and small-for-size syndrome
The clinical features of post-hepatectomy liver failure (PHLF) bear a resemblance to a well-recognized syndrome in liver transplant (LT) practice: the Small-For-Size Syndrome (SFSS).SFSS denotes early graft failure following LT with undersized or partial organs[17,18].Optimal graft-recipient size matching is crucial for LT success, with inadequate grafts typically characterized by a graft-recipient weight ratio of less than 0.8% (GRWR < 0.8%) or a graft-native liver weight ratio of less than 40%[33-36].Undersized grafts fail to meet postoperative metabolic demands, resulting in organ dysfunction marked by hyperbilirubinemia,coagulopathy, and refractory ascites.Sepsis often complicates SFSS, leading to alarmingly high mortality rates[36].While the etiology of SFSS is multifactorial, both graft and recipient factors contribute.Persistent elevated perfusion pressures and portal hypertension post-revascularization are implicated in SFSS-related organ injury, underscoring the complex interplay between graft and recipient factors in the development of this syndrome[37].
Mechanisms involved in the development of small-for-size syndrome
There is an agreement in attributing the cause of this syndrome to portal hyper-inflow[18], manifesting through various mechanisms:
● Shear Stress: Elevated portal pressure in the reduced-size liver induces mechanical trauma at the endothelial level, leading to extensive sinusoidal damage, endothelial cell destruction, and microhemorrhages at portal triads[36].
● Relative Decrease in Arterial Blood Supply: Compared to portal flow, reduced arterial blood supply compromises hepatocyte regeneration, hindering metabolic support crucial for regeneration[38,39].
Itoet al.demonstrated a significant incidence of SFSS in living donor liver transplantation (LDLT),particularly with left lobe partial grafts, correlating with portal pressure[40].Portal vein pressure exceeding 20 mmHg post-LDLT predicts high morbidity and poor graft functional recovery.
Small for size syndrome treatment
Glanemannet al.conducted experiments demonstrating that diverting portal flow significantly enhances outcomes in animal models undergoing 90% liver parenchymal resection[4].Rats subjected to hepatectomy with splenectomy exhibited minimal hepatocyte damage, evidenced by transaminase levels at least three times lower than controls.This improvement was attributed to reduced portal hyperflow post-surgery,evident just 15 min after the procedure, with rates notably lower in the study group (3.5 ± 0.4 mL/min)compared to controls (5.4 ± 0.4 mL/min).Portal diversion also enhances hepatic artery blood flow via HABR activation, arterializing liver-directed blood flow[4].Treatment of SFSS aims to reduce the portal overflow that is characteristic of this syndrome, which is achievable through various portal diversion methods.
DEFINITION OF PORTAL VEIN FLOW DIVERSION AND TYPES OF PROCEDURES
Portal vein flow diversion encompasses procedures aimed at redirecting a variable portion of portal vein flow towards systemic circulation, directly targeting portal hypertension.These procedures include:
● Ligation or embolization of the splenic artery[41,42]
● Splenectomy[36]
● Preemptive portal branch ligation or embolization before hepatectomy, promoting compensatory hypertrophy and enhancing potential functional reserve[43]
● Porto-Systemic Shunts (PSS): including portocaval and splenorenal shunts[44-46]
The primary objectives of these interventions are twofold.Firstly, to diminish portal inflow by splenic artery embolization or ligation, addressing the significant yet fluctuating splenic component of portal hypertension.This approach has proven effective in managing esophageal variceal bleeding and small-forsize syndrome (SFSS), with reported post-surgical reductions in splenic flow of up to 52%[47,48].
Alternatively, diversion of portal blood flow can be achieved through PSS.
Both surgical and radiological portosystemic shunt procedures create a circuit allowing portal blood to bypass the liver, reducing both flow and portal pressure.
Transjugular Intrahepatic Portosystemic Stent Shunt (TIPSS) involves connecting an intrahepatic portal branch to a hepatic vein via a conduit, positioned percutaneously using interventional radiology.Advancements in this radiological method, particularly using covered stents, have improved outcomes in TIPSS patients, reducing interest in surgical shunts[49].However, TIPSS may lead to hepatic encephalopathy and hinder future liver interventions due to the intrahepatic conduit.While indicated for cirrhotic patients with recurrent variceal bleeding and refractory ascites, TIPSS is contraindicated in those with HCC.Thus, it is not suitable for managing portal hypertension during HCC hepatectomy[50].
Surgical portosystemic shunts
The portocaval anastomosis, known as the Eck fistula, first described by T.E.Starzl in 1983[51], rapidly decompresses the portal system and achieves immediate decompression of the portal vein vascular bed[44-48].Subsequently, various types of portosystemic shunts (PSS) have been described.These include connections between portal vein and caval systems through anastomoses between tributary vessels, with or without interposition of human iliac grafts from deceased donors or synthetic vascular prostheses made of Dacron or Goretex?-PTFE (Polytetrafluoroethylene).
Common surgical portosystemic shunts include:
● End-to-side portocaval shunts
● Mesenteric-caval shunts (with prosthesis interposition)
● Proximal (Linton procedure), central (Cooley procedure), and distal (Warren procedure) splenorenal shunts
● Speno-caval shunt (Orozco procedure)
● Side-to-side portocaval shunts, with or without interposition graft/prosthesis (H-graft portocaval shunt)These procedures alter portal hemodynamics, reducing portocaval pressure gradients, but may cause varying degrees of portal flow inversion, depending on shunt type and dimension.
End-to-side shunts result in total portosystemic shunting with no remaining hepatopetal flow.It is associated with the development of refractory ascites in 5% of cases.The bleeding from rupture of esophageal varices is reduced to 5% after such interventions, but the rates of hepatic encephalopathy (which can reach 40%) and impaired liver and heart function (with possible development of high-flow heart failure)are quite high.Nowadays, it is almost abandoned, and it is only used in emergency settings due to its easy technical feasibility[52,53].
Mesenteric-caval and central splenorenal shunts, although effective, are considered secondary choices due to anastomoses on smaller, thrombosis-prone vessels.These procedures are preferred in the setting of portal hypertension due to portal vein thrombosis in non-cirrhotic patients[54-56]; in this setting, especially in pediatric extrahepatic portal vein occlusion, a modified mesenteric-caval shunt, named Meso-Rex Shunt,can be applied[57].
Warren procedure selectively targets esophageal varices, leaving portal flow largely unaffected[56,58-60].
Side-to-side portocaval shunts, whether H-shaped with graft/prosthesis interposition or not, are favored for their simplicity and efficacy in decompressing the portal system.These shunts offer flow calibration to reduce steal syndrome[61-63], and hepatic encephalopathy risk without compromising effectiveness or liver function.The H-graft interposition shunt preserves hepatopetal flow by approximately 80% with low encephalopathy rates (about 5%), and 5% rebleeding from gastroesophageal varices, with shunt patency of about 95% over 7 years[56,58,64,65].Figure 1 provides a comparative overview of outcomes for the main portosystemic shunting techniques.
APPLYING THE PORTOSYSTEMIC SURGICAL SHUNT TO LIVER RESECTION
In cirrhotic patients with HCC, treatment strategy hinges on a delicate balance between tumor-related and cirrhosis-related factors, profoundly impacting patient prognosis[1].Essentially, the severity of cirrhosis diminishes the significance of HCC for long-term survival, prioritizing tumor control over disease clearance.Additionally, cirrhosis poses constraints on surgical options, heightening susceptibility to postprocedural or drug-induced liver failure.The barcelona clinic liver cancer (BCLC) staging system[66]initially developed and validated for HCC management, has become somewhat static over time, particularly inadequate for intermediate and advanced stages and decompensated cirrhotic patients due to evolving medical management and tumor biology understanding[67,68].Increasing evidence demonstrates differences between BCLC recommendations and real-life approaches in HCC treatment[69,70].In response to the limitations of the BCLC system, alternative staging concepts and treatment stage migration strategies have emerged, but these still focus on stage-oriented HCC treatment strategies[71].
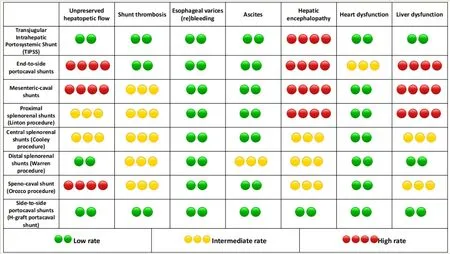
Figure 1.Visual comparison of various portosystemic shunt techniques alongside their primary pathophysiological consequences.
A novel patient-oriented approach, termed “therapeutic hierarchy,” prioritizes treatment feasibility assessment to determine the optimal therapy for each patient at each stage[72,73].
Clinically significant portal hypertension (CSPH), often indicated by imaging findings of splenomegaly,varices, ascites, or a platelet count < 100,000/mL[74], marks decompensated cirrhosis and has historically contraindicated hepatic resections.However, cirrhotic patients with CSPH and HCC within Milan criteria[75]or extended validated criteria[76-79]stand to benefit most from liver transplantation (LT)[72,80].If contraindications to LT arise, these patients, excluded from potentially curative treatments, often receive loco-regional therapy (LRT) or best supportive care (BSC), both yielding dismal prognoses.Despite longstanding contraindications, many tertiary hepatobiliary centers have successfully performed hepatectomy in cirrhotic patients with portal hypertension, reporting acceptable mortality rates, favorable long-term outcomes, and oncologic benefits[81-84].Portal hypertension is not prognostic for perioperative mortality or long-term survival, according to multivariable analyses[83].Moreover, updated guidelines from the European association for the study of the liver (EASL)[1]endorse liver resection in the presence of portal hypertension for patients at low risk of liver decompensation post-surgery[85].
Drawing lessons from LT complicated by SFSS, portal flow diversion strategies, such as portosystemic shunts, may prevent PHLF and expand the boundaries of liver surgery, increasing the number of those who can access hepatectomy with curative intent[86]or as a part of a wider treatment strategy that considers LT a second-line treatment.These shunts reduce sinusoidal wedge pressure post-hepatectomy, potentially preserving residual organ function and enhancing regenerative capacity while minimizing intra- and postoperative morbidity, including bleeding and ascites-major components of PHLF.Intraoperative bleeding, coagulopathy, and new onset ascites are indeed some of the major challenges cirrhotic patients face when undergoing surgery, and the mortality rates have been described as high as 10%-57%[87].Portosystemic shunts have proven safe and effective in facilitating major abdominal surgery in cirrhotic patients.In the first pioneering experiences, it has been noted that patients with previous portocaval shunt performed better following non-hepatic surgery as compared to those without[88,89].In the era of expandedpolytetrafluoroethylene (e-PTFE) covered stents, TIPSS occlusion rates dropped markedly, as well as the incidence of post-procedural hepatic encephalopathy when smaller stents were applied[90-92].These results pushed surgeons to explore non-standard TIPSS applications more.Nowadays, both surgical shunt and TIPSS have been shown to increase the resection rate of gastrointestinal tumors in cirrhotic patients without increasing complication rates, and with less incidence of decompensated ascites after surgery[93-97].In particular, TIPSS followed by surgery after a 30-day interval showed good portal hypertension control, 100%planned surgery completion rate, ascites and encephalopathy both in 12.5% of cases, and 80% overall survival at 1 year[98].However, the TIPSS procedure is difficult to reverse in case of inefficacy or complications[90,92], with poor cost-effectiveness in this scenario[99].Notably, the first case of liver resection for HCC in a patient who had previously placed a TIPSS for decompensated cirrhosis was recently published, and an uneventful postoperative course was reported[100].Nonetheless, TIPSS has several contraindications related to high peri-procedural bleeding and cancer dissemination risk, particularly in HCC patients.Conversely, surgical shunts afford full control of the operating site, minimizing risks.In other words, when TIPSS is contraindicated, surgical portosystemic shunts are still an option.
Expanding liver resection to patients with CSPH serves as both a downstaging strategy before LT and the best alternative for those ineligible for LT, potentially enhancing overall survival in this population[2,72].
Technical aspects of liver resection with portocaval shunt
In liver surgery in general, but even more so in HCC, it is necessary to consider the extent of hepatic resection (minor resection versus major resection) based on the number of liver segments to be removed.It is now clear that preoperative assessment of hepatic resection safety relies on FRL volume and liver function, but safety limits for hepatic resection remain a debated issue in the literature.In the scenario we have described, and based on previous evidence, we suggest performing a surgical shunt when hepatic resection in a cirrhotic patient exceeds 40% of the total liver volume (FRL < 60%)[101].
A different issue concerns the theme of anatomical resections compared to non-anatomical resections.The evidence available so far suggests that non-anatomical hepatic resection can lead to an ischemic area in the residual part of the adjacent liver with a higher amount of debris from the resection edge; this increases the risk of infectious complications in the postoperative course[102].The cirrhotic patient with portal hypertension is more exposed and susceptible to infectious events, so it is useful to minimize this risk in every phase, including the surgical procedure.Since anatomical resection is associated with less debris from the resection site, we recommend this type of procedure when deciding to perform a surgical portosystemic shunt.
One potential drawback of expanding the HCC resection pool through liver resection preceded by a surgical portocaval shunting is the requirement for an open abdomen procedure.However, minimally invasive approaches for HCC resection in cirrhotic patients have shown a more favorable outcome, with lower rates of blood transfusion and complications compared to open surgery[103,104].Nevertheless, in highly selected cases where clinically significant portal hypertension (CSPH) limits access to liver resection as a potentially curative treatment or as part of a downstaging protocol, performing a calibrated portocaval shunt before liver resection has been described[86].Our group has demonstrated the safety and effectiveness of this technique in selected cases, as evidenced by our case series results [Table 1] [Figure 2].Remarkably, a patient underwent LT four years after liver resection and remains free of HCC recurrence, even eight years post-surgery (four years post-LT).
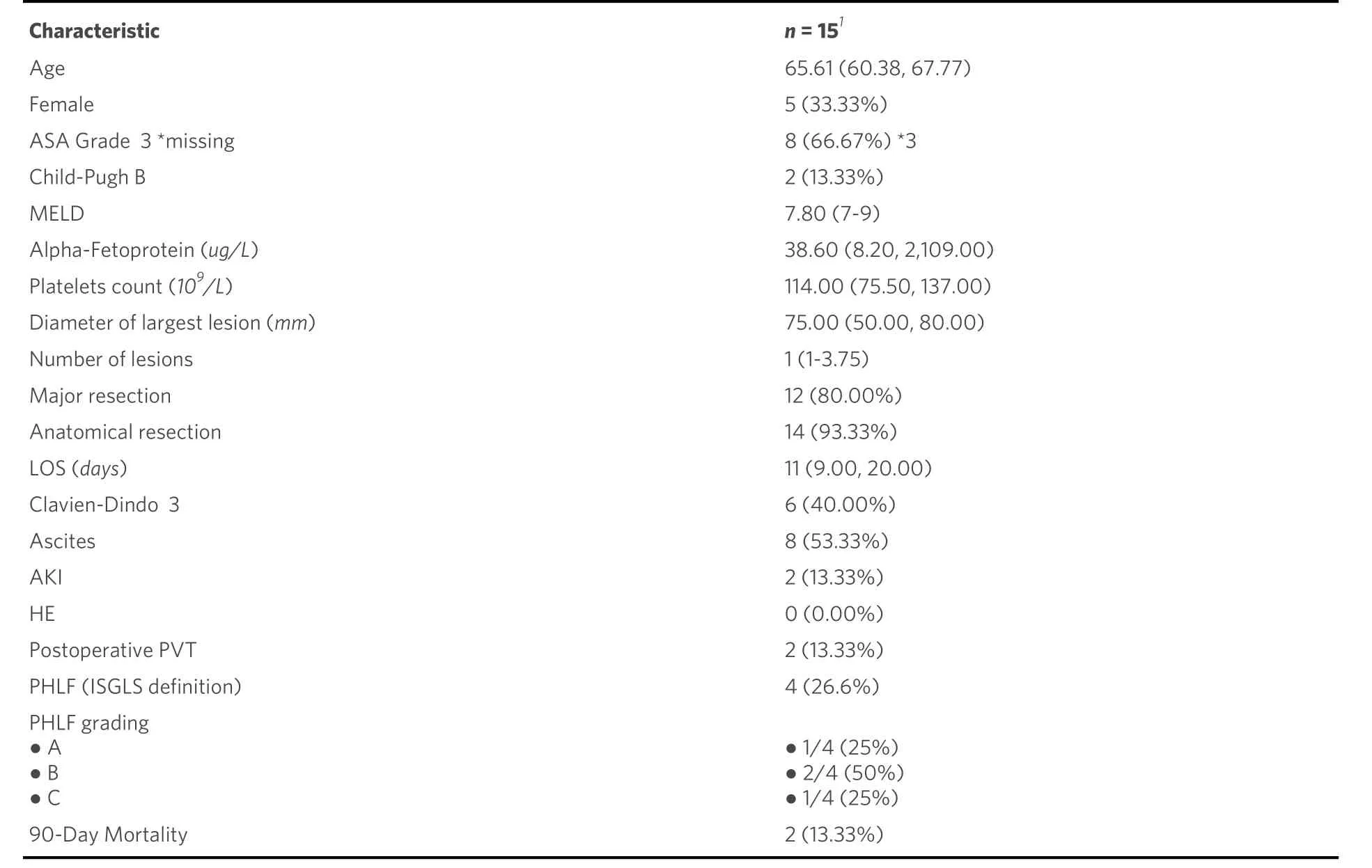
Table 1.Case series of 15 liver resections for HCC on cirrhosis with portocaval shunt during surgery.Demographic characteristics,disease burden, type of surgery, and postoperative outcomes.(Unpublished data, Author’s personal experience)
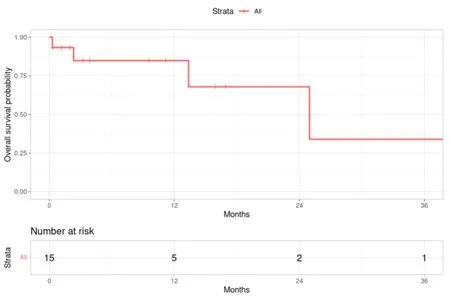
Figure 2.Kaplan-Meier survival curves of 15 HCC patients who underwent liver resection with H-graft portocaval shunt.Overall survival rates at 1, 2, and 3 years were 84.8%, 67.9%, and 33.9%, respectively (unpublished data, Author’s personal experience).
Surgical technique
H-graft portocaval shunt
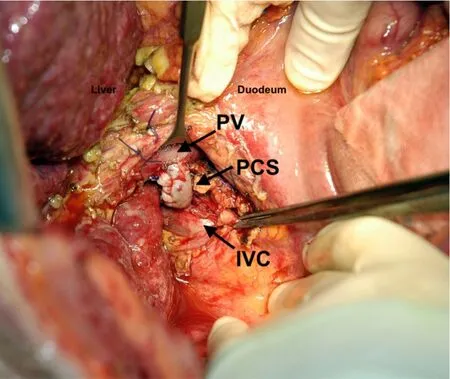
Figure 3.During surgery in a patient from the authors' series, an intraoperative photograph depicts the H-graft portocaval shunt constructed using a free iliac vein graft.(PV portal vein, PCS portocaval shunt, IVC inferior vena cava).
Surgical exposure is achieved by a transverse upper abdominal or reverse “L” incision.Retrograde cholecystectomy is performed, and the hepatoduodenal ligament is approached.Dissection of the retroportal lymph nodes is carried out to expose the portal vein and common bile duct.Careful dissection is carried out to allow for medial retraction of the common bile duct, and the right hepatic artery, in case of aberrant anatomy of the latter.The axis of the portocaval shunt and the portal vein should be parallel for the technical success of the shunt.Hence, an oblique incision should be made on the inferior vena cava (IVC).Caudate lobectomy or transection of the caudate process might be required to expose a sufficient length of the IVC and to achieve the desirable orientation, which, along with sufficient mobility of the portal vein,assures a tension-free anastomosis.For H-type shunts, we opt for a 0.6 cm diameter Goretex? vascular prosthesis; eventually, free iliac cadaveric vein graft of compatible blood group.In the latter scenario, the cadaveric vein graft is surgically calibrated to 6 mm [Figure 3].The portocaval shunt is carried with partially occluding vascular clamps (Satinsky) and 6-0 running Prolene suture.Intraoperative Doppler ultrasound is carried out at the completion of the shunt to check the portal, arterial, and shunt flows.If necessary,invasive measurement of portal pressure is carried out (with the use of a 25-G needle attached to a water pressure gauge with saline).
Pathophysiological consequences of the surgical portacaval shunt
The surgical portocaval shunt presents certain pathophysiological consequences owing to its efficacy and rapid hemodynamic alterations.Competition for portal flow between the remnant liver and the shunt may lead to organ failure due to hypoperfusion[105].This diversion of blood flow into the systemic circulation reduces pressure both at the sinusoidal level and in the portal vein, as well as within the collateral circulation.However, a surgical portosystemic shunt utilized in liver resection may be functionally temporary.As the future liver remnant (FLR) regenerates, the sinusoidal vascular bed re-establishes,potentially leading to spontaneous late thrombosis of the shunt when no longer required.Nevertheless,these benefits may be accompanied by complications such as transient exacerbation of liver function and hepatic encephalopathy, with side-to-side portacaval shunts more prone to such issues compared to H-graft shunts[45,106].Consequently, the H-graft shunt is the Authors’ procedure of choice.
In cases of persistent encephalopathy unresponsive to medical treatment, closure of the surgical shunt may be considered once liver regeneration is complete[45,105].
CONCLUSIONS
Portal flow diversion and surgical portosystemic shunts in patients with CSPH present an intriguing avenue for expanding the indications for liver resection in select HCC patients once deemed unresectable due to portal hypertension-associated risks of postoperative liver failure.Advanced liver cirrhosis and portal hypertension should not be viewed as absolute contraindications for liver resection.Instead, they warrant individual evaluation for each patient, weighing the survival benefits offered by available treatment options on a case-by-case basis.This evaluation process should occur within a multidisciplinary framework to ensure comprehensive and tailored management strategies.
DECLARATIONS
Authors’ Contributions
Performed the literature research and wrote the paper: Lanari J, Polacco M Designed the paper and reviewed the final draft: Cillo U
Availability of data and materials
Author data are only available upon appropriate and reasoned request.
Financial support and sponsorship
None.
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
Patients’ data were handled in accordance with the ethical guidelines of the 2013 revised Declaration of Helsinki.Each patient signed a consent for every procedure performed in the hospital, and for the collection and use of data anonymously for research and publication purposes, and all procedures were performed in accordance with the Declaration of Istanbul.No one received compensation or was offered any incentive.
Consent for publication
All patients sign an informed consent at the presentation in which they agree to collect and use their personal data anonymously for research purposes.
Copyright
? The Author(s) 2024.
- Hepatoma Research的其它文章
- Introduction of Chinese expert consensus on neoadjuvant therapy for primary liver cancer (2023 edition)
- Introduction to 2023 Chinese expert consensus on the whole-course management of hepatocellular carcinoma
- Reflections and perspectives on adjuvant treatment in the setting of resected hepatocellular carcinoma
- Dysmetabolic comorbidities and non-alcoholic fatty liver disease: a stairway to metabolic dysfunctionassociated steatotic liver disease
- Progression of liver disease and associated risk of hepatocellular carcinoma
- The role of percutaneous hepatic perfusion (PHP) in the treatment of cholangiocarcinoma

